Chapter 6. Non-Parenteral Medication Administration
6.3 Administering Medications by Mouth and Gastric Tube
Medication by Mouth
Medication is usually given orally, which is generally the most comfortable and convenient route for the patient. Medication given orally has a slower onset and a more prolonged, but less potent, effect than medication administered by other routes (Lynn, 2011).
Prior to oral administration of medications, ensure that the patient has no contraindications to receiving oral medication, is able to swallow, and is not on gastric suction. If the patient is having difficulty swallowing (dysphagia), some tablets may be crushed using a clean mortar and pestle for easier administration. Verify that a tablet may be crushed by consulting a drug reference or a pharmacist. Medications such as enteric-coated tablets, capsules, and sustained-release or long-acting drugs should never be crushed because doing so will affect the intended action of the medication. Tablets should be crushed one at a time and not mixed, so that it is possible to tell drugs apart if there is a spill. You may mix the medication in a small amount of soft food, such as applesauce or pudding.
Position the patient in a side-lying or upright position to decrease the risk of aspiration. Offer a glass of water or other oral fluid (that is not contraindicated with the medication) to ease swallowing and improve absorption and dissolution of the medication, taking any fluid restrictions into account.
Remain with the patient until all medication has been swallowed before signing that you administered the medication.
Checklist 44 outlines the steps for administering medication by mouth.
Disclaimer: Always review and follow your hospital policy regarding this specific skill. |
|||
Safety considerations:
|
|||
Steps |
Additional Information |
||
| 1. Check MAR against doctor’s orders. |
Check that MAR and doctor’s orders are consistent.  Night staff usually complete and verify this check as well. |
||
2. Perform the SEVEN RIGHTS x 3 (must be done with each individual medication):
Medication calculation: D/H x S = A (D or desired dosage/H or have available x S or stock = A or amount prepared) |
The right patient: check that you have the correct patient using two patient identifiers (e.g., name and date of birth). The right medication (drug): check that you have the correct medication and that it is appropriate for the patient in the current context. The right dose: check that the dose makes sense for the age, size, and condition of the patient. Different dosages may be indicated for different conditions. The right route: check that the route is appropriate for the patient’s current condition. The right time: adhere to the prescribed dose and schedule. The right reason: check that the patient is receiving the medication for the appropriate reason. The right documentation: always verify any unclear or inaccurate documentation prior to administering medications.  NEVER document that you have given a medication until you have actually administered it. |
||
3. The label on the medication must be checked for name, dose, and route, and compared with the MAR at three different times:
|
 These checks are done before administering the medication to your patient. If taking drug to bedside (e.g., eye drops), do third check at bedside. |
||
| 4. Place all medications that patient will receive in one cup, except medications that require pre-assessment (e.g., blood pressure or pulse rate). Place these in a separate cup and keep wrapper intact. | Keeping medications that require pre-assessment separately acts as a reminder and makes it easier to withhold medications if necessary. | ||
| 5. Do not touch medication with ungloved hands. Use clean gloved hands if it is necessary to touch the medication. | Using gloves reduces contamination of the medication. | ||
| 6. Circle medication when poured. | Pour medication. Circle MAR to show that medication has been poured.
 |
||
7. Patient education
|
The patient has the right to be informed and provided with reasons for medication, action, and potential adverse effects. Giving this information will likely improve adherence to medication therapy and patient reporting of adverse effects.
Confirms patient’s allergy history. |
||
| IMPORTANT: If patient expresses concerns over medications, do not give medication. Verify doctor’s order and explore patient concerns before administering medication. | |||
8. Positioning
|
 Correct positioning reduces risk of aspiration during swallowing. Water or other oral fluids will help with swallowing of medication. Proper body mechanics reduces risk of injury to health care provider. |
||
9. Administer medication orally as prescribed.
|
Follow any specific descriptions for administration of the medication.
Wear gloves if placing the medication inside the patient’s mouth.
|
||
10. Post-medication safety check
|
Do not sign for any medications if you are not sure the patient has taken them.
Post assessments determine effects and potential adverse effects of medications. |
||
| 11. Return within appropriate time to evaluate patient’s response to the medications and to check for possible adverse effects.
If patient presents with any adverse effects:
|
Most sublingual medications act in 15 minutes, and most oral medications act in 30 minutes.
|
||
| Data source: BCIT, 2015; Lilley et al., 2011; Perry et al., 2014 | |||
Medication via a Gastric Tube
Patients with a gastric tube (nasogastric, nasointestinal, percutaneous endoscopic gastrostomy [PEG], or jejenostomy [J] tube) will often receive medication through this tube (Lynn, 2011). Liquid medications should always be used when possible because absorption is better and less likely to cause blockage of the tube. Certain solid forms of medication can be crushed and mixed with water prior to administration.
Checklist 45 outlines the steps for administering medication via a gastric tube.
Disclaimer: Always review and follow your hospital policy regarding this specific skill. |
|||
Safety considerations:
|
|||
Steps |
Additional Information |
||
| 1. Check MAR against doctor’s orders. | Check that MAR and doctor’s orders are consistent.
 Night staff usually complete and verify this check as well. |
||
2. Perform the SEVEN RIGHTS x 3 (must be done with each individual medication):
Medication calculation: D/H x S = A (D or desired dosage/H or have available x S or stock = A or amount prepared) |
The right patient: check that you have the correct patient using two patient identifiers (e.g., name and date of birth).
 The right medication (drug): check that you have the correct medication and that it is appropriate for the patient in the current context. The right dose: check that the dose makes sense for the age, size, and condition of the patient. Different dosages may be indicated for different conditions. The right route: check that the route is appropriate for the patient’s current condition. The right time: adhere to the prescribed dose and schedule.  The right reason: check that the patient is receiving the medication for the appropriate reason. The right documentation: always verify any unclear or inaccurate documentation prior to administering medications. NEVER document that you have given a medication until you have actually administered it. |
||
3. The label on the medication must be checked for name, dose, and route, and compared with the MAR at three different times:
|
 These checks are done before administering the medication to your patient. If taking drug to bedside (e.g., eye drops), do third check at bedside. |
||
| 4. Place all medications that patient will receive in one cup, except medications that require pre-assessment (e.g., blood pressure or pulse rate). Place these in a separate cup and keep wrapper intact. | Keeping medications that require pre-assessment separately acts as a reminder and makes it easier to withhold medications if necessary. | ||
| 5. Do not touch medication with ungloved hands. Use clean gloved hands if it is necessary to touch the medication. | Use gloves to reduce contamination of medication. | ||
| 6. Circle medication when poured. | Pour medication. Circle MAR to show that medication has been poured.
 |
||
7. Patient education:
|
The patient has the right to be informed, and providing reasons for medication, actions, and potential adverse effects will likely improve adherence to medication therapy and patient reporting of adverse effects.
Confirm patient’s allergy history. |
||
| IMPORTANT: If patient expresses concern about medications, do not give medication. Verify doctor’s order and explore patient concerns before administering medication. | |||
| 8. Help patient to a high sitting position unless contraindicated. | This position reduces risk of aspiration during swallowing. | ||
| 9. Determine if medication should be given with or without food. If the medication is to be given on an empty stomach, the enteral feeding may need to be stopped from 30 minutes before until 30 minutes after the medication is given. | Follow specific medication guidelines to ensure adequate absorption and distribution of the medication. | ||
| 10. Apply clean non-sterile gloves. | Using gloves prevents spread of microorganisms. | ||
| 11. Check gastric tube for correct placement as described in Chapter 10. | Ensure that tube is properly placed prior to administering medication to prevent aspiration. | ||
| 12. Dilute medication in 15 to 30 ml of water. | Dilution keeps the tube from blocking. | ||
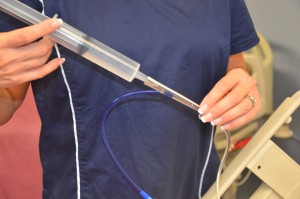
| 13. Remove plunger from a 60 ml gastric tube syringe and attach syringe to the end of the gastric tube while pinching the gastric tube. | Make sure the tip of the syringe fits the end of the gastric tube. | ||
| 14. Pour medication and water solution into the 60 ml syringe, release pinch, and allow fluid to drain slowly by gravity into the gastric tube. | If fluid does not drain by gravity, gentle pressure may be applied using the plunger of the syringe, but do not force the medication through the tube.
 |
||
| 15. Flush 10 ml of water between medications. | This step prevents interactions between medications. | ||
| 16. After the last medication has been given, flush the tube with 30 ml of water. | Flushing prevents blocking of the tube. | ||
| 17. Keep the patient in a high sitting position to prevent aspiration. | This position prevents aspiration and encourages absorption of medication. | ||
18. Post-medication safety check:
|
Post assessments determine effects and potential adverse effects of medications. |
||
| 19. Return within appropriate time frame to evaluate patient’s response to the medications and to check for possible adverse effects.
If patient presents with any adverse effects:
|
Evaluate patient for intended and adverse effects. | ||
| Data source: BCIT, 2015; Lilley et al., 2011; Perry et al., 2014 | |||
Critical Thinking Exercises
- Your patient is dysphagic. Discuss the steps you should take and the considerations you should be cognizant of to administer oral medication safely.
- Your patient is receiving medication and nutritional sustenance via an enteral gastric tube. The drug reference guide recommends that the medication you should administer be given without food. Discuss how you would approach this situation to ensure the safe administration of the medication.