Acute Care Content in HCA Courses
Health Care Assistants in Acute Care
The addition of acute care content in the current Health Care Assistant Program Curriculum Guide (2015) is at the level of introducing students to the acute care context only, and only in theory and lab courses. Practice experiences in acute care are not part of the 2015 Guide.
With a goal of minimizing disruption to the 2008 curriculum (to not require a change in hours or a shift in existing content from one course to another), the following table indicates where acute care content could fit into existing courses with associated outcomes/content and align with the HCA Program Curriculum Guide (2015). Time estimates for the added content are also given.
The acute care content provided in this section is based on materials developed by Island Health[1] (formerly Vancouver Island Health Authority, VIHA). Instructors are encouraged to adapt and integrate this content into their instructional activities (e.g., PowerPoint slide, student handouts, course manuals, etc.).
| Content Added | Courses and Strategies | Time Added |
|---|---|---|
| 1. The supervision structures in acute care that support HCA practice | Health Care Assistant: Introduction to Practice | 30 minutes |
| 2. Similarities and differences between clients in acute care settings and clients in residential or community settings | Healing 1: Caring for Individuals Experiencing Common Health Challenges | 1 hour 30 minutes |
| 3. Specific elements of the acute care environment | Healing 1: Caring for Individuals Experiencing Common Health Challenges
Healing 3: Personal Care and Assistance |
No additional time |
| 4. How the role of the HCA may change in the acute care setting, depending on client acuity and intensity | Healing 1: Caring for Individuals Experiencing Common Health Challenges | 1 hour |
| Health Care Assistant: Introduction to Practice course | 15 minutes | |
| Health and Healing: Concepts for Practice | 30 minutes | |
| 5. Key considerations for providing holistic, person-centred care for acute care clients with IV lines, tubes, wounds, and surgical incisions | Healing 3: Personal Care and Assistance | 2 hours theory/lab |
| 6. Strategies for prioritizing tasks, demonstrating flexibility in work assignments, problem-solving and decision-making regarding care provision | Health and Healing: Concepts for Practice
Healing 1: Caring for Individuals Experiencing Common Health Challenges Healing 3: Personal Care and Assistance |
1 hour theory/lab |
| 7. Interprofessional collaborative practice in acute care settings | Health Care Assistant: Introduction to Practice | No additional time |
| 8. The importance of knowing when and how often to communicate with the client and health care team | Healing 1: Caring for Individuals Experiencing Common Health Challenges (specific examples related to acute care)
Healing 3: Personal Care and Assistance (specific examples/applications related to acute care) Health Care Assistant: Introduction to Practice (concepts related to supervision) |
30 minutes |
| 9. The role of the HCA in responding to emergency codes | Health and Healing: Concepts for Practice
Healing 3: Personal Care and Assistance (apply to lab scenarios) |
30 minutes |
| 10. Other acute care revisions | Healing 2: Caring for Individuals Experiencing Cognitive or Mental Challenges | 15 minutes |
Acute Care Content in HCA Courses
1. The supervision structures in acute care that support HCA practice
Course: Health Care Assistant Introduction to Practice
Estimated additional time: 30 minutes
Examples of content based upon Island Health materials
- Every health authority and unit has an organizational structure. This organizational structure outlines the supervision structure by identifying who reports to whom.
- Within a unit structure, there are members of the health care team that will guide the role of the HCA. This includes the team members who the HCA will report to when supporting client care and/or unit operations. These team members may include, but are not limited to, Registered Nurses (RNs), Licensed Practical Nurses (LPNs), Registered Psychiatric Nurses (RPNs), Clinical Nurse Leads (CNLs) and Unit Managers.
- Supervisors can help determine which team members HCAs will regularly work with.
- Depending on who assigns and delegates the tasks, different team members need to establish supervision plans for the activities that HCAs will support.
- Communication is essential when reporting to and collaborating with other members of the health care team.
- As an HCA, there will be times where different types of questions and concerns should be brought to different members of the health care team. HCAs can also talk to their unit supervisors/leaders for guidance.
2. Similarities and differences between clients in acute care settings and clients in residential or community settings
Course: Healing 1: Caring for Individuals Experiencing Common Health Challenges, specifically within Learning Outcome #4: Ways to organize, administer and evaluate person-centred care. The content could be addressed with case studies or other activities already being delivered in teaching the course by basing some of these in acute care to emphasize differences.
Estimated additional time: 1 hour 30 minutes
Examples of content based on Island Health materials
- In most instances, acute care settings will be very different from residential and home or community care settings. The pace of activities and the variety of sights, sounds, and smells can be overwhelming for someone new. However, in much the same way as we view a beehive, all of this activity is purposeful and coordinated. All interprofessional team members work collaboratively in a variety of different ways in order to meet many diverse client and family care needs every day.
- As HCAs become acquainted with the acute care setting, they will start to notice that in many instances acute care and residential care settings will share the same clients along their health and wellness journey. Many of these clients will be elderly clients who have been admitted into acute care units for some type of medical intervention, such as surgery, or to deal with a chronic condition that requires symptom control or readjustment. The care needs of these types of clients will be very familiar to HCAs who have practised in other settings. It is within these instances that HCAs can offer significant support to these clients, families, and other members of the health care team.
- There are some important considerations to keep in mind when HCAs are working in an acute care setting. The first is that HCAs will never be working independently. Instead, HCAs will draw upon the knowledge, skills, and resources of a variety of interprofessional care team members that will work collaboratively with them in caring for each client. Secondly, as a member of the interprofessional care team, HCAs also bring with them a wealth of knowledge and skills in caring for elderly clients. These skills and knowledge in caring for the elderly add strength to the interprofessional team and can contribute to the care planning process.
- Acute care is a complex working environment. HCAs have many skills that contribute to providing quality care in this setting, but may not be familiar with some of the unique aspects of the acute care environment.
- As part of a process of exploring how skills translate from residential or community settings, we will look at what might be the same and what might be different about working in acute care.
- It is important to note that the role of the HCA may vary from site to site and from health authority to health authority.
- Residential and community-based clients may be admitted to acute care in the following circumstances. If the client:
- Is frail, elderly, and has a fractured hip
- Has had a stroke or a heart attack
- Has acute congestive heart failure
- Has uncontrolled pain
- Requires surgical intervention
- Has a crisis in their caregiving supports
- Most clients in acute care will have different medical needs than those in residential or community settings. For example, they may:
- Have had recent surgery
- Have lines and tubes
- Have new incisions, wounds, or dressings
- Be experiencing acute mental health issues
- Be admitted for alcohol and drug detoxification
- Be acutely palliative
3. Specific elements of the acute care environment
Course: Healing 1: Caring for Individuals Experiencing Common Health Challenges; applied aspects in Healing 3: Personal Care and Assistance
Estimated additional time: covered in #2 and #5
Examples of content
Examples of environmental aspects more often encountered in the acute care setting may include:
- Additional forms of documentation, or documentation the HCA will access more often than they might in other settings
- Increased technology, such as various pumps, monitors, etc.
- Positive/negative pressure rooms for isolation
- Call bell systems
4. How the role of the HCA may change in the acute care setting, depending on client acuity and intensity
Course: Healing 1: Caring for Individual Experiencing Common Health Challenges; may be addressed through specific examples while teaching about specific health challenges. Acute care information should also be added to Learning Outcome #1: “Display an understanding of the roles…” in the Introduction to Practice course
Estimated additional time: 1 hour in Common Health Challenges, 15 minutes in Introduction to Practice, and 30 minutes in Concepts for Practice (recording/reporting)
Examples of content based on Island Health materials
- HCAs can help care for clients in the acute care setting by helping with:
- Bathing and washing
- Toileting
- Meal assistance
- Basic treatments (as identified by site-specific role and responsibilities)
- Ambulation, mobilization, and transfer of stable clients
- The health care professional (Registered Nurse, Social Worker, Speech Language Pathologist, etc.) considers such factors as client stability and impact/probability of an adverse event prior to assigning tasks. HCAs are generally assigned tasks where the impact/probability of an adverse event is lower. The health care professional will modify their supervision plan depending on these factors.
- Introduce the concepts of acuity and intensity.
- High acuity clients are those who experience an event that is characterized by sharpness or severity, having a sudden onset, sharp rise and short course and lasting a short time. Examples of clients with high acuity needs are those with:
- Respiratory distress (using high flow oxygen)
- Active gastrointestinal bleeding
- Unstable vital signs
- Low acuity clients are those who have become more stable in their health concerns, the prescribed medical treatment is working, and they are demonstrating improvements in their health status. Examples of clients with low acuity care needs are those:
- Who are progressing as expected, three days after an operation
- With pneumonia, requiring IV antibiotics
- With influenza (the flu)
- With C. difficile
- Intensity refers to the volume of work that may be required from the health care team to meet the care needs of a particular client. Examples of clients with high intensity/complex care needs are those who require:
- Complete ADL support — total care client
- Care of more than one health care team member (e.g., mechanical lifts, bariatric clients, etc.)
- Complex wound management (e.g., VAC dressings, ulcers, infected surgical wounds, etc.)
- Support to manage complex family dynamics
- Examples of clients with low intensity/complex care needs are those who require:
- Minimal ADL support required for client care
- Basic meal tray set up (clients who are able to feed themselves)
- Limited support as they are stable and waiting to be discharged or transferred
- High acuity clients are those who experience an event that is characterized by sharpness or severity, having a sudden onset, sharp rise and short course and lasting a short time. Examples of clients with high acuity needs are those with:
- Complexity refers to the range of variables, such as multiple medical diagnosis or challenging family dynamics, which may influence the care needs of a particular client.
5. Key considerations for providing holistic, person-centred care for acute care clients with IV lines, tubes, wounds, and surgical incisions
Course: Healing 3: Personal Care and Assistance
Estimated additional time: 2 hours theory/lab
Examples of content based on Island Health materials
- Examples of lines and tubes in acute care are:
- Intravenous lines
- Oxygen tubing
- Surgical drains
- Chest tubes
- NG tubes
- Catheters
- How do these lines and tubes affect the care of acute care clients?
- Considerations for giving daily care, such as removing or putting on new gowns.
- Asking the RN if there is anything special that they need to know or do related to this client’s tubing.
- Receive instructions from the RN/LPN about any special approaches or care plan interventions.
Emphasize: When providing care, be sure to look at the client and to look at the site of the surgical or medical line. Seek assistance if there are any concerns or questions before proceeding with care and care-related activities.
IV lines
Ask: “What is an IV?”
Answer: An intravenous catheter is a small plastic cannula that is inserted in the vein with the use of a needle. After the plastic cannula is secure within the vein, the needle is removed. They are most commonly inserted in the hand or forearm but can be located in other areas such as the foot. Intravenous catheters are used to supply a client with additional fluids or medications.
Ask: “What does an HCA need to do when providing care to a client with an IV?”
Answer: When providing care to a client with an IV, the HCA should:
- Never remove the IV bag from the pole it is situated on.
- Never disconnect a tube or unplug equipment from the wall without having permission from the RN to do so.
- Notify an RN if:
- They observe blood in the IV tubing or the IV site is leaking.
- They accidentally dislodge the IV during care.
- The client is complaining about pain in the area.
- Avoid getting the dressing or insertion site wet during care.
- If available, use an IV gown to dress the client (IV gowns will have snaps on the sleeves of the gown).
- Check with the RN or team leader about specific client information or instructions before mobilizing a client. Clients who are allowed to be up and walking and have an IV can generally be mobilized.
- There are a few exceptions.
Oxygen tubing
Ask: “What does an HCA need to know about providing care to a client with oxygen tubing?”
Explain: Clients may require oxygen therapy as either a short-term intervention (clients with pneumonia, for example) or for long-term use (such as COPD clients). How much oxygen therapy is required and what method of delivery is used will depend on the client’s condition and may change as the client improves or deteriorates. Chronic conditions, such as COPD, will require consistent oxygen therapy at all times.
Describe: Different methods of delivering oxygen, such as nasal prongs or facial masks.
Ask: “What does an HCA need to do when providing care to a client on oxygen?”
Answer: When providing care to a client on oxygen, the HCA should:
- Never adjust the flow rate of the oxygen.
- Check with the RN or team leader about whether the client requires oxygen before and during mobilization.
- Check with the RN or LPN If you find oxygen tubing laying on the floor in rooms where there is more than one client, to ensure that the nasal prongs are replaced before being reapplied to the correct client.
- Reapply nasal prongs to a client if the prongs become dislodged during care.
- Check with the RN or team leader about specific client information before mobilizing a client.
- Clients who are ambulatory and on oxygen generally can be mobilized.
- There are a few exceptions.
Surgical drains
Ask: “What is a surgical drain?”
Answer: Surgical drains are:
- External drainage systems that are used to collect and drain internal fluids after a surgical procedure.
- There are many different types of surgical drains, and HCAs must always confirm instructions with the health care team prior to providing care for clients with surgical drains.
- Often pinned to gowns to prevent them from accidentally becoming dislodged.
- Often covered by dressings.
Ask: “What does an HCA need to do when providing care to a client with a surgical drain?”
Answer: When providing care to a client with a surgical drain, the HCA should:
- Use caution when removing a client’s gown, as some drains may be pinned to the gown.
- Safely remove safety pins from the old gown and secure them to the new gown when care is complete.
- Never remove a dressing that may be oozing. HCAs may place a gauze over the site and must report it to the RN or team leader immediately.
- Avoid getting the dressing around the drain wet during care. Wash and dry around the dressing site.
- Report any pain or discomfort a client may experience during care and care-related activities.
- Read the client’s care plan/talk to their RN or your team leader to determine if the client is allowed to sit/get up and walk if they have a surgical drain. HCAs should also have the RN or team leader check the client prior to getting out of bed to ensure the drainage system is secure.
Chest tubes
Ask: “What does an HCA need to know about providing care to a client with a chest tube?”
Answer: HCAs need to know that:
- Chest tubes are used when a client’s lung cannot inflate and deflate on its own. This may be the result of an external trauma such as an accident, or as a result of a fluid buildup in the lung that has caused it to collapse.
- Chest tubes are secured with a lot of tape.
Ask: “What does an HCA need to do when providing care to a client with a chest tube?”
Answer: When providing care to a client with a chest tube, the HCA should:
- Avoid getting too much moisture around the chest tube dressing. Wash around the tape with a moist washcloth.
- Report any drainage that may be observed during care to the RN or team leader.
- Report any pain or discomfort a client may experience during care and care-related activities.
- Always check with the RN prior to mobilizing a client with a chest tube. Accidently dislodging or withdrawing the chest tube may cause the client to go into respiratory distress and requires immediate medical intervention.
Catheters
Ask: “What does an HCA need to know about providing care to a client with a catheter?”
Answer: HCAs need to know that:
- Catheters in acute care settings are inserted as a short-term medical intervention. This may include surgical clients both pre-operatively and post-operatively to facilitate bladder drainage during surgery. Unless otherwise indicated, catheters in acute care settings should only be used for short periods of time.
- Although clients who are allowed to be up and walking and have catheters can generally be mobilized, there are a few exceptions. HCAs must check with the RN or team leader about specific client information.
Ask: “What does an HCA need to do when providing care to a client with a catheter?”
Answer: When providing care to a client with a catheter, the HCA should:
- Confirm instructions and gather information regarding anything that may be different in providing care for a specific client with a catheter.
- Report any pain or discomfort a client may experience during care or care-related activities.
Surgical incisions
Ask: “What types of surgical incisions would you expect to see in acute care?”
Answer: In acute care, you may encounter a wide variety of incisions. Incisions are generally covered with a dressing/bandage.
Common surgical incisions include:
- Abdominal incisions
- Hip or knee incisions
- Other
Ask: “What does an HCA need to do when providing care to a client with a surgical incision?”
Answer: When providing care to a client with a surgical incision, the HCA should:
- Confirm instructions with the RN/LPN.
- Gather information and supplies for care.
- Seek permission from the client to look at the bandage over the incision and to perform care.
- Notify an RN immediately if there is a large amount of drainage on the bandage over the incision.
- Never remove a dressing that may be oozing. HCAs may place a gauze over the site and must report it to the RN or team leader immediately.
- Avoid getting a dressing wet during care. Wash and dry around the dressing site.
- Report any pain or discomfort a client may experience during care and care-related activities.
6. Strategies for prioritizing tasks, demonstrating flexibility in work assignments, and problem-solving and decision-making regarding care provision
Course: Health and Healing: Concepts for Practice; Healing 1: Caring for Individuals Experiencing Common Health Challenges; applied aspects in Healing 3: Personal Care and Assistance
Estimated additional time: 1 hour for theory/lab
Examples of content based on Island Health materials
Ask: “What does an HCA need to know to prioritize tasks when providing care in acute care settings?”
Answer: When providing care in acute settings, HCAs need to know that:
- Acute care environments and client assignments can change rapidly due to:
- Client admissions and discharges
- Moving clients from one room to another
- Transferring clients from one unit to another
- Changing acuity of clients
- Clients developing infections that require special precautions
The health care team needs to respond to these changes by managing their priorities.
Ask: “What does an HCA need to do to prioritize tasks when providing care in acute care settings?”
Answer: When providing care in acute care settings, HCAs need to:
- Attend huddles/shift reports or seek information from the other members of the health care team about changing priorities throughout the day.
- Seek guidance and direction from the RN or LPN related to their responsibilities.
- Communicate clearly with the health care team to identify what tasks have or have not yet been completed.
- Anticipate that they will need to be flexible in their client care assignment based on the clients’ needs. Although they may have been given assignments, they may be reassigned during their work days due to unforeseen circumstances.
Emphasize that although HCAs may not be assigned to specific client assignments or teams, they may be required to support specific aspects of daily care under the direction of another health care team member. This will require a level of flexibility and adaptability of the HCA to meet the client care needs in the rapidly changing environment in acute care.
Problem-solving and decision-making regarding care provision
Case studies or lab scenarios could be used to give students an opportunity to apply critical thinking and problem-solving skills to acute care settings, or to compare and contrast acute care and other settings.
7. Interprofessional collaborative practice in acute care settings
Course: Health Care Assistant Introduction to Practice
Estimated additional time: not applicable, as already covered in program
Interprofessional collaborative practice is important because it meets the following needs in providing client care:
- Improving client outcomes, care, and services
- Reducing medical error
- Ensuring knowledge transfer and communication between, and to, relevant professionals
- Informing government policy and leadership at all levels
- Addressing health and human resource shortages
Describe: When teams work interprofessionally:
- Decision-making is shared
- Leadership is shared
- The role of each health care provider is understood and the client and family are included in the process
- Team communication is efficient, open, respectful, and client-centred and the client and family are integrated into the care process
Highlight: The outcomes of interprofessional collaboration.
Clients and families have:
- Expressed more satisfaction and identified a more positive experience
- Enhanced self-care and health condition knowledge and skills
- Improved health outcomes
- More timely referrals to other team members
- More comprehensive care
Health care providers:
- Are more satisfied and have a more positive experience
- Develop enhanced knowledge and skills
- Experience improved communication between providers
The health care system:
- Can offer a broader range of services and more efficient use of resources
- Provides improved access to services and shorter wait times
- Improves coordination of care
Reference: Barrett, J., Curran, V., Glynn, L., & Godwin, M. (2007). CHSRF synthesis: interprofessional collaboration and quality primary healthcare. Canadian Health Services Research Foundation.
8. The importance of knowing when and how often to communicate with the client and health care team
Course: Healing 1: Caring for Individual Experiencing Common Health Challenges; applied aspects in Healing 3: Personal Care and Assistance. This also relates to supervision in Introduction to Practice. Specific examples related to acute care could be included in Healing 1 and Healing 3
Estimated additional time: 30 minutes
Examples of content based on Island Health materials
Communication principles in acute care for HCAs:
- Who to communicate with: know the interprofessional team that is involved in client care
- What to communicate: the methods of gathering, reporting, and recording information
- When to communicate: the urgency and frequency of communication required
- Where to communicate: whiteboards, client charts, huddles, meetings
- Why communication is important
- How to communicate: unit processes and technology
- Communication processes within acute care settings require the full and active participation of all interprofessional team members.
- In acute care, it is important to consider the urgency for information (how quickly something is needed) as well as the frequency required of communication (how regularly information is needed). Critical decisions regarding such factors as hospital admissions and discharges, client care routines, diagnostic assessments, medical treatments, and access to supplies depend on clear and timely communication between team members.
Reinforce the importance of frequent communication in acute care settings.
Emphasize that the other members of the health care team will base their analysis, synthesis, and evaluation of client care on their observations and information (such as care planning or physician’s orders).
Explain that other members of the hospital team will base their client access and flow decisions on the most recent client information (such as who can be discharged or who can be admitted to a room and when).
Identify any specific protocols or site-specific processes that HCAs may encounter that will highlight the need for urgent and frequent communication processes (such as reduced staffing levels and high client acuity levels). Explain what the HCA role and responsibilities will be within these processes (such as re-prioritizing care and care activities to attend to different unit requirements).
Reinforce that HCAs should:
- Report any client care information during regular communication processes (in huddles, for example).
- Report any observations or concerns with client care, such as changes in client condition or bleeding, to the health care team leader immediately.
- Record any client care information they perform, such as bowel record or recording food or fluids, immediately after completing the task.
Emergent or emergency events may occur with a client or with a member of the health care team.
Acknowledge that sometimes communication processes do not go well. Explain the reporting structure that HCAs may use as a guide to facilitate difficult communication processes. Highlight any specific protocols, policies, or procedures that may be used at this site to address ongoing or unresolved communication difficulties (such as respectful workplace policies).
There are several YouTube videos that reinforce the concept of communication
Therapeutic communication for nurses (from a client’s perspective)
Classic Sesame Street – Ernie and Bert can’t communicate
Sesame Street – Ernie and Bert “Very Important Note”
Poor communication (health care assessment – context of care)
“See Me, Nurse” – video clips to the poem about nursing
9. The role of the HCA in responding to emergency codes
Course: Coverage recommended in the Health and Healing: Concepts for Practice course. A lab scenario could also be added into the Healing 3: Personal Care and Assistance course
Estimated additional time: 30 minutes
Review the role of the HCA in assisting with emergencies
The following lists are examples of what may be expected of HCAs for the three top codes at one particular site:
Code Blue:
- Activate help (this may simply involve notifying the unit clerk, LPN, or RN nearest to the phone system, or emergency call button).
- Remove all obstructions from the client’s bedside and room (bedside table, chairs, etc.).
- Close the privacy drapes of any clients in the same room.
- Stand in the hallway and direct emergency personnel to the correct room.
- Be available to retrieve supplies and equipment that the code response team may require.
- Comfort any clients who may be located in the same room.
- Clean and tidy the area after the event.
Explain the site policy and protocol for both witnessed and unwitnessed cardiac arrests.
Code White:
A call for help due to a potentially violent situation, or a violent or escalating incident.
- Call for help (this may simply involve notifying co-workers, the unit clerk, LPN, or RN nearest to the phone system or emergency call button). 911 may have to be called.
- Maintain personal safety at all times, removing yourself and any clients who may be at risk.
- Be available to provide support to those responding to the code white.
- Seek first aid if you were injured.
- Participate in any review of the incident.
- Provide support to those who may have been affected by the incident. Be aware of your own internal responses to the event and seek help if you are experiencing unhealthy reactions.
- Recognizing that a member of the interprofessional care team may not be available as a resource for HCA practice during the time they are responding to an event, identify the next appropriate care provider who will provide guidance and direction.
Question: What are the differences between a code white response in a hospital, residential care home, and in a community setting?
Code Yellow:
- Activate help (this may involve notifying the unit clerk, LPN or RN nearest to the phone system).
- Seek direction from the interprofessional care team.
- Join unit team members in the systematic search of the unit.
- Be specific and thorough in your search processes.
- Report back to the RN or team leader as soon as your area has been searched to receive further direction.
Content is covered by online orientation for students doing placements at health region sites.
Code Red:
Content is covered in the online orientation for students doing placements at health region sites.
Standardized codes in B.C.
The following codes have been standardized for B.C. Not all codes will be used by all health regions or all sites.
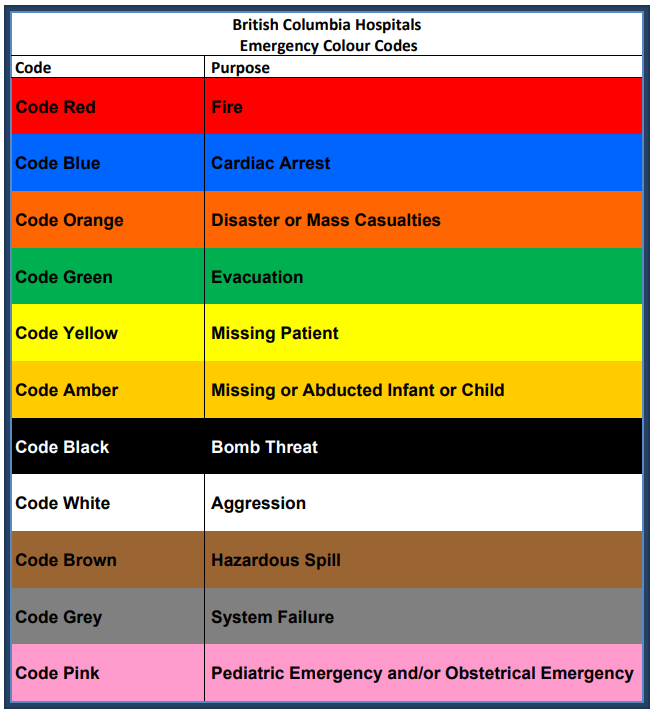
Refer to the following document for further information:
Ministry of Health Services Policy Communiqué: Standardized Hospital Codes
10. Other acute care content revisions
Course: Healing 2: Caring for Individuals Experiencing Cognitive or Mental Challenges
Estimated additional time: 15 minutes
Examples of content based on Island Health materials
Explain: There are specific criteria and processes for people who are admitted involuntarily into acute care.
An involuntary admission is guided by criteria that are outlined in the Mental Health Act of British Columbia.[2] Generally, the client has been examined by a physician who is of the opinion and provides reporting supporting the opinion that the client:
a. Has a mental health disorder.
b. Requires treatment in or through a designated facility.
a. Requires care, supervision, and control in or through a designated facility to prevent the person’s or patient’s substantial mental or physical deterioration or for the protection of the person or patient or the protection of others.
b. Cannot suitably be admitted as a voluntary patient.
Reinforce that depending on specific client care needs, there may be unique forms that are being used by the health care team. An example of client needs is substance withdrawal – CIWA protocol.
Image descriptions
British Columbia Hospitals Emergency Colour Codes
- Code red: fire
- Code blue: cardiac arrest
- Code orange: disaster or mass casualties
- Code green: evacuation
- Code yellow: missing patient
- Code amber: missing or abducted infant or child
- Code black: bomb threat
- Code white: aggression
- Code brown: hazardous spill
- Code grey: system failure
- Code pink: pediatric emergency and/or obstetrical emergency
- Island Health Authority, the B.C. Health Education Foundation and the Ministry of Health Services are acknowledged for granting permission to adapt material from the Island Health Transitional Learning Continuum, Health Care Assistant in Acute Care Curriculum (2012). ↵
- Mental Health Act [RSBC 1998] Chapter 288, Section 22. http://www.bclaws.ca/civix/document/id/complete/statreg/96288_01#section22 ↵

