Healing 3: Personal Care and Assistance
Course Guideline
A minimum of 65% of this course should consist of the supervised application of hands-on skills to ensure students are deemed safe and competent in performing personal care.
Suggested Learning Strategies
Strategies that Focus on Caring
1. Personal Care Discussion
Use the following questions and statements to elicit discussion about caring:
- Discuss this statement: Careful and consistent handwashing is one of the most caring things you can do for yourself and your client. (Consider: Diseases like norovirus may have short-term effects for workers, but be fatal to clients).
- How is being concerned about safety related to caring? (Consider: Your safety and the safety of your client are linked. If you are hurt physically or psychologically, the care that you provide will be affected. If you are injured, you won’t be there to provide care at all).
- What are some ways an HCA can show caring while assisting a client with hygiene and grooming? With moving and ambulation?
- In what ways can an HCA show caring while assisting a client with elimination?
- How is being concerned about accuracy in measuring vital signs related to caring? How is being meticulous when assisting with medications, or when carrying out a delegated task, related to caring?
2. Scenarios from Clinical Situations
Use scenarios from clinical situations to help students contextualize the caregiving practices they are learning in this course. With only preliminary information about the client who is the recipient of care, ask students to consider the following:
- What further information should be collected prior to commencing care for a client? Where and from whom should information be gathered?
- What should be included in a quick assessment of the client prior to providing care or assistance? Why?
Once the student has collected information and assessed the (simulated) client, they will progress with the provision of care or assistance. During this process, the student should be observed to assure that:
- Adequate communication with the client takes place (and family, if appropriate).
- The client’s comfort and independence are appropriately maintained.
- The client’s privacy and dignity are maintained.
- The client’s preferences are honoured as much as possible.
- The care or assistance provided is consistently safe for both the client and the student.
- The care or assistance is provided in an organized manner.
Following the provision of care or assistance, the student will be invited to reflect on the process using the points above and to discuss their experience with those who observed the process.
3. Unfolding Case Study: Caring for Peter Schultz
As a homework assignment, have students review their client portfolio for Peter Schultz.
- Whole Class Review
- In class, ask students to summarize what they have learned about Peter, highlighting details related to his personal history and family, health care services accessed in community and residential care, and his health status.
- Small Group Discussion
- Divide the class into small groups. Have the students read the following scenario describing changes to Peter’s health status and response to care. Students will then use the STUDENT HANDOUT below to objectively record the observations that have been made. For each observation, the students should list possible responses that fall within the parameters of the HCA role.
- Whole Class Activity
- Come back together as a class and ask the groups to share the observations and responses that were identified, highlighting what should be reported to the team leader. Following this, lead the students in a discussion about possible interventions or adaptations to the plan of care that may be made by a health care professional, based on the observations that have been reported by the HCA. Emphasize how observations shared by HCAs advocate for the client, support a collaborative team approach, and lead to safe and effective client care. If time allows, the instructor may decide to develop or update a care plan for this client as a classroom activity.
STUDENT HANDOUT
Unfolding Case Study: Caring for Peter Schultz
Changing Client Health Status and Response to Care
DIRECTIONS: Read the following scenario. Then populate the table with observations based on the situation provided. For each observation, list possible responses that fall within the parameters of the HCA role.
You are an HCA who has been working at the same residential care home for the past five years. Today is your first day back after a two-month absence, and you are assigned to care for Peter Schultz. As you carry out the plan of care, you observe changes in Peter’s health status and response to care.
You have always enjoyed providing care for Peter. When he first moved to the care home four years ago, you used several strategies to include him in the morning care routine. He especially enjoyed singing old tunes and reciting poems while you were helping him to get ready for the day. He enjoyed his meals and was a regular participant in the music and exercise programs and daily social hour. You always appreciated Peter’s smile and hearing him laugh.
Since Peter has moved to the care home, he has been diagnosed with Alzheimer’s disease, in addition to the diagnosis of vascular dementia following a CVA. He now requires full assistance with his activities of daily living and is on a regular toileting schedule. Over the past year, Peter’s legs have gotten weaker and he is no longer able to bear weight. He is on medication for blood pressure and bowel control.
Over the past year, Peter has become progressively less responsive during the morning care routine. He says very little and usually just listens as you sing his favourite songs. You have also observed that he smiles less often. Usually, when you try to involve him in simple care- related activities, such as washing his face or combing his hair, he will reach out for the face cloth or hair brush that you offer him, but will not use them unless you guide his hands for him. This morning when you offer him the face cloth, he does not reach out his hand to take it.
Since losing his ability to walk, Peter has used a wheelchair to ambulate. The foot pedals on his chair are removed and he uses his feet or the side rail to move himself up and down the hallway. Today when you look for Peter to bring him to the lunch room, you notice that he has not moved from the place where he was one hour ago. When you assist Peter with his lunch, he doesn’t try to hold his cup as he used to. He eats very slowly and clears his throat often. You observe that he finishes half of his mashed potatoes, but coughs when you offer him small pieces of minced chicken. He eats all of his chocolate pudding. It takes Peter 55 minutes to eat his lunch.
This afternoon, Eve comes to attend a special music program with Peter. When you walk with her to his room, you find that he has fallen asleep in his chair. Eve tells you that Peter has fallen asleep every day after lunch for the past two weeks. Eve has a difficult time waking Peter up to listen to the guest musicians. It takes an hour for Peter to drink a cup of thickened coffee and when Eve gives him a cookie, it drops out of his hand.
| Observation | HCA Response |
|---|---|
| Peter did not reach out to take the face cloth when it was offered to him. | Continue to offer the face cloth to Peter. If he does not reach out for it, place it in his hand and guide him in washing his face. Minimize distractions during this care activity. Continue to monitor Peter’s response to this approach. |
Metzger, Z.B. (2010). The Last Lap of the Long Run, Addendum to “On the Long Run”: An Account of our Travels with Dementia. This material is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License (CC BY-SA 4.0).
Download Student Handout: Changing Client Health Status and Response to Care [PDF].
Strategies that Focus on Critical Thinking, Problem-Solving, and Decision-Making
1. Classroom Debate Activity
Invite students to engage in a debate about a topic discussed in this course. Divide the class into small groups of three to five students and assign two groups to each of the topics outlined; one group will take a pro position towards the topic and the other group will take a con position.
Ask each group to identify two to three reasons to support the position they have been assigned. Then, with the instructor acting as the moderator, the two groups will engage in a debate using the following structure:
- Each group provides a brief introduction to their position on the topic.
- In alternating format, the two groups present the two or three reasons identified to support their position.
- Each group provides a brief closing statement.
After the debate has concluded, briefly come together as a larger group and summarize the positions that were presented. Invite feedback from the students not involved in the debate and discuss further considerations. Alternate groups until each student has participated in a debate.
Debate topics for Healing 3: Personal Care and Assistance.
- Past experiences with a client should influence future care provided to that client.
- Restraints should not be used in residential care settings.
2. Critical Thinking Exercises
After students have learned about body mechanics and asepsis, and have mastered basic transfer, bathing, and toileting techniques, present them with scenarios that simulate various practice environments, such as community (homelike) settings and acute care. Working in small groups of two or three, students should use critical thinking, problem-solving, and decision-making skills to consider how they will apply the skills in settings that are different from the standard lab setting or in changing situations.
Situations may include:
- Home settings, such as one that would be found in an apartment: very small bathrooms, low beds, low and soft chairs. Encourage students to identify situations in which safety is NOT possible without changes in the environment or the assistance of another health care worker or a mechanical lift.
- Acute care settings where clients may have wound dressings, IVs, or other tubes.
- Less medically stable clients (e.g., client has pain while being repositioned in bed or becomes dizzy and weak while being transferred to a chair). Ask students what actions they will take (reporting immediately, recording).
- A witnessed cardiac arrest while providing care (e.g., summoning help, commencing CPR if trained and per employer policies, being available to assist the team as directed).
3. Case Study: Putting Safety into Practice
The following case study is used with permission of Island Health[1].
The case study, provided as a STUDENT HANDOUT below, could be used as a “pen and paper” exercise, either individually or with the students in small groups, or it could be set up as a practice scenario. There is also a DISCUSSION GUIDE below on putting safety into practice.
Note the use of the four-step process to help ensure patient safety:
- Prevent
- Actions and measures put in place to minimize the chances of a safety event occurring.
- Check
- Prepare yourself, the environment and others before proceeding with the task.
- Respond
- Actions taken to eliminate or minimize an identified safety risk.
- Report
- Let others know about safety concerns or incidents.
STUDENT HANDOUT
Putting Safety into Practice[2]
DIRECTIONS: Read the scenario and make notes to consider how to best provide safe care using the four-step process to ensure patient safety.
Mary is a new HCA working on a general medicine unit.
She is about to go into Mr. Lee’s room to assist him to the bathroom for morning care. Mr. Lee shares his hospital room with one other gentleman.
Mary confirms instructions for morning care with the RN and finds out from his chart that Mr. Lee requires stand by assistance with his mobility and wears a gait belt[3] while he is walking. Mary confirms that she will observe and supervise while Mr. Lee moves from a sitting to standing position and while he walks from his bed to the bathroom.
Mary begins to set up the space. She gathers towels, a change of hospital gown, and toiletries. She looks for his gait belt but cannot find one next to his bed. She notes there is one hanging by his roommate’s closet door.
Keeping in mind a standard process, Mary considers the “Prevent, Check, Respond, and Report” steps.
- Prevent – What actions or measures should Mary put in place to minimize the chance of a safety event?
- Check – How should Mary prepare herself, the environment, and others before proceeding with the task?
- Respond – What actions should Mary take to eliminate or minimize an identified safety risk(s)?
- Report – What and to whom should Mary report about safety concerns or incidents?
Download Student Handout: Putting Safety into Practice [PDF].
DISCUSSION GUIDE
Putting Safety into Practice
- Prevent
- Wanting to prevent spread of infection, Mary gets a new gait belt from the clean supply storage area and uses gloves during care.
- Mary washes her hands both before and after assisting with care.
- Check
- Mary checks with the chart to see if Mr. Lee has special precautions to follow (e.g., gowning).
- She checks how she is feeling – able to focus? Able to perform safe body mechanics?
- Using her health authority’s pre-mobility check (e.g., cognition, cooperativeness, and physical ability), Mary confirms no changes to patient abilities from what the RN reported.
- She checks to make sure the pathway to the bathroom is clear of clutter and safe to walk.
- She ensures that the bed is at a good height to make it safer for Mr. Lee to go from sit to stand.
- As per his chart, Mr. Lee has a gait belt on in case she needs to provide support.
- Respond
- After determining it is safe to proceed, Mary closely watches Mr. Lee as he gets up and walks. She is ready to call for help if required.
- Report
- Mr. Lee was able to walk to the bathroom and perform his own care with minimal support or direction. Mary reports this to the RN.
- Mary knows that if Mr. Lee did have a slip or fall, she would follow her site’s procedures to report on this event.
Download Discussion Guide: Putting Safety into Practice [PDF]
Strategies that Focus on Professional Approaches to Practice
1. Handling Challenging Situations
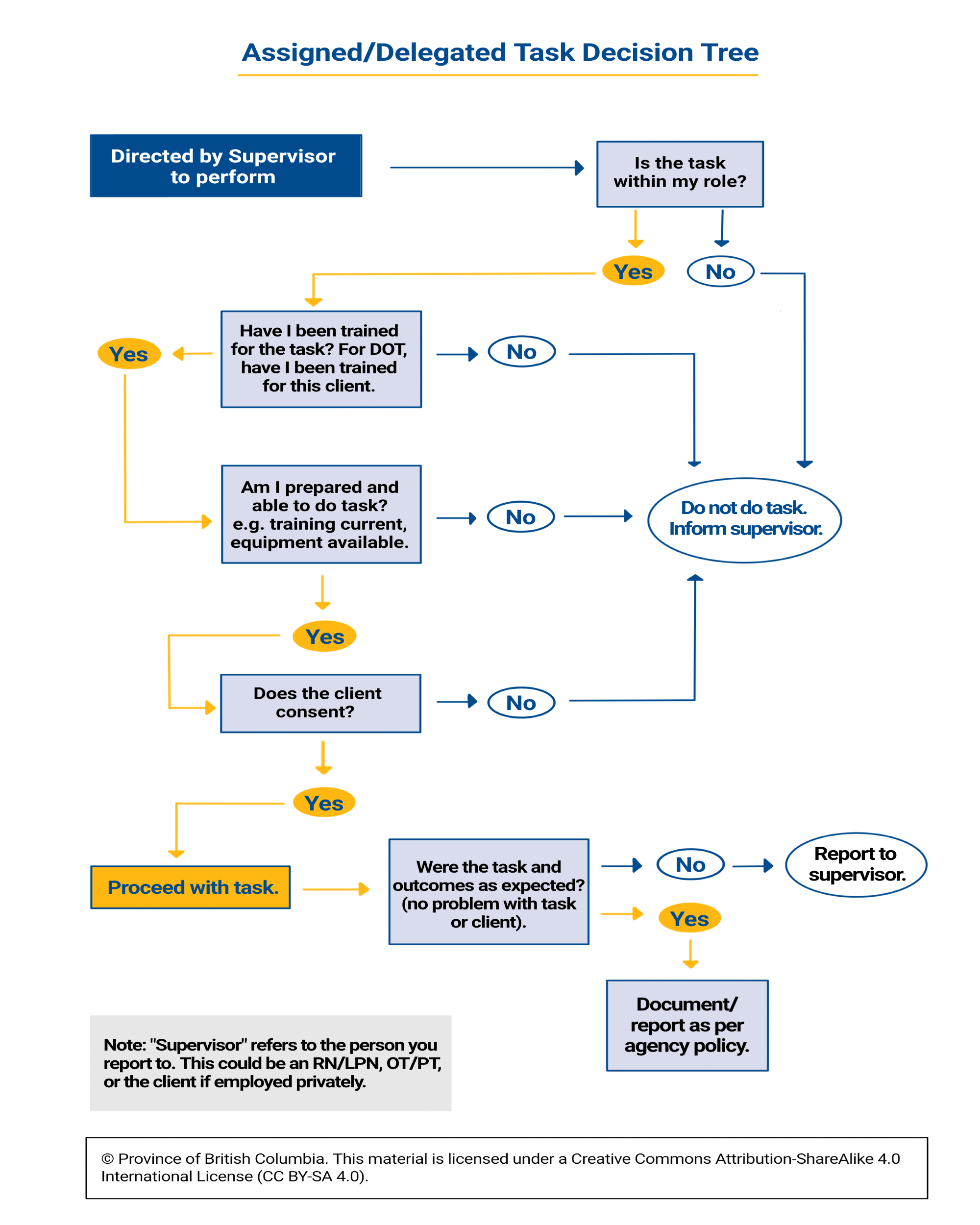
Invite students, working in small groups, to discuss scenarios in which, as HCAs, they are faced with being asked to undertake questionable activities. For each one, have them identify an appropriate response and explain their response. Suggest that they refer to the Assigned/Delegated Task Decision Tree for support during this activity.
Here are some examples:
As an HCA, you are providing care and service for an elderly gentleman, Mr. Syms, who requires help with his meals and his bath. One day, when you arrive at Mr. Syms’ house, you find that a doctor is visiting him. Apparently, Mr. Syms’ daughter, who lives across town, called the doctor when her father complained of chest pain. The doctor says to you, “Well, he seems to be fine now. Maybe it was only indigestion.” As he is leaving, he says to you, “Mr. Syms was telling me that his back is bothering him. I’ve left some Tylenol with codeine. Give him two of those whenever he needs them.”
How might you handle this situation?
As an HCA, you have been visiting Mr. and Mrs. Sihota for several months. Mrs. Sihota is a woman of 78 years who is physically frail and experiencing some cognitive decline. Two days ago, she had day surgery to correct a cataract in her left eye. Mr. Sihota is almost 10 years older than his wife and suffers from arthritis and heart problems.
When you come to their house, Mr. Sihota greets you at the door saying, “Thank goodness you are here. Now you can give my wife her eye drops. I’m no good at that sort of thing and she’ll be happier to have you do it.”
How might you handle this situation?
You are working on an acute care orthopaedic ward. When you walk into the room of a client you have not met before, he says, “Oh, there you are, nurse. Can you please hand me the magazine that’s on the chair?”
Student Self-Assessment Video Scenarios
The following video scenarios have been developed for students to self-assess their learning prior to their practice experience. Instructors should provide the links for these videos to their students near the end of the Healing 3: Personal Care and Assistance course so students can complete each scenario and be better prepared for their practice experiences. Instructors should review these videos before assigning them to students.
Instructors can request or require that students submit a reflective journal for each video scenario. Another option is to have a class or small group discussion after all students have completed the video(s). A Self-Assessment Video Reflective Journal Sheet [PDF] sample is available.
Video Scenarios
- Roles and Responsibilities of the HCA
- Communicating with the Health Care Team
- Isolation Precautions
- Lifts and Transfers
- Morning Care
Suggestions for Follow-Up Discussion
There are also some practices and procedures that are worthy of follow-up discussion. For example:
- Roles and Responsibilities of the HCA. In this video, the nurse is wearing a bracelet and an activity tracker on her wrist while administering cream on the client’s back. Wearing a bracelet would normally not be acceptable; however, the bracelet is actually a medical alert bracelet, and she wears the activity tracker to monitor her heart rate. Students could be asked to consider this situation and comment on alternative practices that could be used, such as wearing the bracelet and activity tracker on the non-dominant arm or covering them with a glove.
- Communicating with the Health Care Team. In this video, Mrs. Simon jumps from the past to the present tense when she talks about her wife. Trevor does not correct Mrs. Simon on these details, but instead redirects and engages her in a meaningful activity by asking her about the pictures, etc. Students could be asked to reflect on Mrs. Simon’s actions and words and determine if they truly reflect those of a client with Alzheimer’s disease.
- Isolation Precautions. Institutions may use isolation signs that differ from the ones used in this video. Students could be directed to comment on the use of various isolation signs and discuss what is acceptable and not acceptable.
- Lifts and Transfers. Practices for lifts and transfers may vary from facility to facility. The students could be asked to comment on the practices outlined in this video. For example, students can discuss whether a gait belt should be used for Mrs. Barclay, and if so how they would go about getting this added to the client’s care plan.
- Morning Care. Bathing a client can be done in a variety of ways as long as principles are maintained. Students could comment on whether Edgar proceeded in a manner that followed principles of hygiene. They could discuss what could have been done differently.
Suggested Course Assessments
The course learning outcomes may be assessed by the following tasks:
- One or more quizzes or examinations that pertain to principles, legal/defined parameters of practice, and safety in relation to the implementation of personal care and assistance skills (Learning Outcomes #1, #3, and #4).
- Demonstrations of ability in performing personal care and assistance skills that maintain the comfort and safety of the client and the safety of self and other members of the health care team. Students should be checked on their competency in performing specific skills by their instructors. Peer review and using skills checklists may also be useful for formative assessment as students seek to develop their proficiency (Learning Outcomes #1, #2, #3, and #4). Refer to Section 5: Sample Evaluation Tools.
- Prior to the first clinical experience, demonstration of skills performance through an integrated skills practice examination (scenario-based lab skills assessment). Students should demonstrate their ability to:
- Perform personal care and assistance skills competently.
- Maintain the comfort and dignity of the client.
- Maintain the safety of the client, self, and other members of the health care team.
- Perform in an organized manner.
- Maintain medical asepsis.
- Utilize proper body mechanics.
- Communicate with the client and other health care team members where appropriate.
Testing can be accomplished through performance of a scenario simulating the practice environment and may include an opportunity for problem-solving. The specific skills tested and expected level of competency may vary, depending upon when the first clinical experience occurs within the program. At a minimum, students should perform safely prior to entering the clinical setting. Students should be evaluated using clear and consistent criteria; an evaluation rubric may be used (Learning Outcomes #1, #2, #3, and #4). Refer to Section 5: Sample Evaluation Tools.
- Completion of a safety assessment in a home environment. Preferably, students would conduct this assessment as part of their community care (home support) practice experience (See STUDENT HANDOUT Home Safety Assessment Guide below.) The questions included in this assessment are not definitive; the program may adapt this tool, as necessary. Based on the assessment, the student should discuss the safety issues that they have identified and make suggestions for ways that the environment could be made safer for the client/family and members of the health care team (Learning Outcomes #2 and #4).
- Completion of a reflective journal assignment to confirm students have viewed the self-assessment videos in preparation for clinical (Learning Outcomes #1, #2, #3, and #4).
STUDENT HANDOUT
Home Safety Assessment Guide
DIRECTIONS: In addition to conducting the assessment (indicating with a checkmark where met), make comments on safety issues identified (items unmet) and suggest ways that the environment could be made safer for the client/family and members of the health care team.
General Assessment
|
| Comments: |
Living Room
|
| Comments: |
Kitchen
|
| Comments: |
Bathroom
|
| Comments: |
Bedroom
|
| Comments: |
© Province of British Columbia. This material is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License (CC BY-SA 4.0).
Download Student Handout: Home Safety Assessment Guide [PDF].
Resources for Healing 3: Personal Care and Assistance
Online Resources
B.C. Centre for Disease Control. http://www.bccdc.ca/
B.C. Centre for Disease Control. (2017). Harm reduction guidelines. http://www.bccdc.ca/health-professionals/clinical-resources/harm-reduction
B.C. Centre for Disease Control & Government of British Columbia, Ministry of Health. (2020, August 31). Infection prevention and control requirements for COVID-19 in long-term care and seniors’ assisted living. http://www.bccdc.ca/Health-Info-Site/Documents/COVID19_LongTermCareAssistedLiving.pdf
B.C. Public Service Agency and B.C. Government & Services Employees Union (2007). Guide to Prevention and Control of Infectious Diseases in the Workplace. https://www2.gov.bc.ca/assets/gov/careers/managers-supervisors/managing-occupational-health-safety/infectious_disease_guide.pdf
Doyle, G. R. & McCutCheon, J. A. (n.d.). Ostomy care. In Clinical procedures for safer clinical care. BCcampus. https://opentextbc.ca/clinicalskills/chapter/10-6-ostomies/
Fortis B.C. (2017). Gas leaks and odours. https://www.fortisbc.com/safety-outages/natural-gas-safety/gas-leaks-and-odour
Government of British Columbia. (n.d.). Safety at home. https://www2.gov.bc.ca/gov/content/family-social-supports/seniors/health-safety/safety-at-home
Government of British Columbia, Ministry of Health Services. (2008). Personal assistance guidelines. https://www.health.gov.bc.ca/library/publications/year/2008/Personal_Assistance_Guidelines.pdf
Interior Health. (2017). Safe patient handling videos. https://www.interiorhealth.ca/sites/Partners/WHSresources/Pages/SafePatientHandling.Aspx
Provincial Infection Control Network of British Columbia. https://www.picnet.ca/
Provincial Residential Care Musculoskeletal Injury Prevention Team (2011). Provincial safe resident handling standards for musculoskeletal injury prevention in British Columbia. https://www.safecarebc.ca/wp-content/uploads/2020/10/Provincial-Safe-Resident-Handling-Standard-2011.pdf
SafeCareBC. (n.d.). Point of care risk assessment. http://safecarebc.ca/wp-content/uploads/Point-of-Care-Risk-Assessment-SCBC-Version1.pdf
Tiner, S. (2020, April 1). Your new super power: Hand-washing. Mayo Clinic. https://discoverysedge.mayo.edu/2020/04/01/your-new-super-power-hand-washing/?_ga=2.139963571.1440117354.1590880017-2090357955.1590880017
WorkSafeBC. (2014). Back talk: An owner’s manual for backs. https://www.worksafebc.com/en/resources/health-safety/books-guides/back-talk-an-owners-manual-for-backs?lang=en
WorkSafeBC. (2009). Controlling exposure: Protecting workers from infectious disease. https://www.worksafebc.com/en/resources/health-safety/books-guides/controlling-exposure-protecting-workers-from-infectious-disease?lang=en
WorkSafeBC. (n.d.). Health care and social services. https://www.worksafebc.com/en/health-safety/industries/health-care-social-services
WorkSafeBC. (2006). Home and community health worker handbook. https://www.worksafebc.com/en/resources/health-safety/books-guides/home-and-community-health-worker-handbook
WorkSafeBC. (2020). Patient handling: Overhead lifts vs floor lifts – what’s the difference? https://www.worksafebc.com/en/resources/health-safety/hazard-alerts/patient-handling-overhead-lifts-vs-floor-lifts?lang=en
WorkSafeBC. (2014). Patient handling. https://www.worksafebc.com/en/health-safety/industries/health-care-social-services/topics/patient-handling
WorkSafeBC. (2020). Patient handling: Soaker pads. https://www.worksafebc.com/en/resources/health-safety/hazard-alerts/patient-handling-soaker-pads?lang=en
WorkSafeBC. (2013). WorkSafeBC occupational health and safety regulations.
Ergonomics (MSI) requirements. https://www.worksafebc.com/en/law-policy/occupational-health-safety/searchable-ohs-regulation/ohs-regulation/part-04-general-conditions
Biological agents. https://www.worksafebc.com/en/law-policy/occupational-health-safety/searchable-ohs-regulation/ohs-regulation/part-06-substance-specific-requirements
WorkSafeBC. (2013). Two person care needs a planned approach. https://www.worksafebc.com/en/resources/health-safety/videos/two person-care-needs-a-planned-approach?lang=en
WorkSafeBC. (2019). WHMIS (Workplace hazardous materials information system). https://www.worksafebc.com/en/health-safety/hazards-exposures/whmis
Online Videos
Align Home Health. (2015, November 17). Glove removal [Video]. YouTube. https://youtu.be/wZO9O9iGlKs
All N One Home Health. (2015, November 12). How to help someone who uses a wheelchair including walkers, crutches and canes [Video]. YouTube. https://www.youtube.com/watch?v=EZestPFcvP0
American College of Surgeons. (2015, September 8). Feeding tube skills: What is an enteral feeding tube? [Video]. YouTube. https://www.youtube.com/watch?v=1Gd_LSR9VIA
Coughsafevideos. (2012, March 7). Why don’t we do it in our sleeves [Video]. YouTube. https://www.youtube.com/watch?v=CtnEwvUWDo0
Dynamis. (n.d.). Bathing without a battle [Video]. Vimeo. https://vimeo.com/121147508
Eaton, C. (2014, August 29). Bed bath and occupied bed making video part 1 [Video]. YouTube. https://www.youtube.com/watch?v=75O-MWF8K6w
Eaton, C. (2014, August 29). Bed bath and occupied bed making video part 2 [Video]. YouTube. https://www.youtube.com/watch?v=zjPu4EbbGNE
FunctionFocusedCare. (2013, June 26). Function focused care for assisted living residents: Dressing [Video]. YouTube. https://www.youtube.com/watch?v=4qTVkBn2i-A
FunctionFocusedCare. (2013, June 26). Function focused care for assisted living residents: Toileting [Video]. YouTube. https://www.youtube.com/watch?v=tNDGfuUtcFo
Globalhygienecouncil. (2012, September 20). Bacteria on your hands [Video]. YouTube. https://www.youtube.com/watch?v=YfzgWpG4H5c
Handicare. (n.d.). Handicare band sling [Video]. Vimeo. https://vimeo.com/269759430
Handicare. (n.d.). Handicare positioning sling [Video]. Vimeo. https://vimeo.com/274733472
Handicare. (n.d.). Handicare TriTurner sling [Video]. Vimeo. https://vimeo.com/269767001
Handicare. (n.d.). Handicare universal sling [Video]. Vimeo. https://vimeo.com/274735676
Handicare North America. (2018, June 29). Handicare slings: ComfortCare [Video]. YouTube. https://youtu.be/NxpHCFBGNuE
Handicare North America. (2018, June 29). Handicare slings: Deluxe hammock [Video]. YouTube. https://www.youtube.com/watch?v=qrcl6TzSM4o
Healthy Canadians. (2020, June 2). COVID-19: How to wear a non-medical mask or face covering properly [Video]. YouTube. https://youtu.be/gvLA–hGU70
Kozak, J. (2012, May 20). How may I help you? – A guide to assisting the visually impaired [Video]. YouTube. https://youtu.be/YS8aaPmZeUI
Lippincott, Williams and Wilkins. (2013, March 25). Positioning and lifting patients and residents [Video]. YouTube. https://www.youtube.com/watch?v=H68Sa04s_1s
Lortie, C. & Fontaine, N. (2022). AM Skills Care [Video]. Selkirk College and College of the Rockies. https://media.bccampus.ca/media/0_m3jtuj4o
Marwaha, S. (2011, September 30). Wash your hands – it just makes sense [Video]. YouTube. https://www.youtube.com/watch?app=desktop&v=M8AKTACyiB0
Ostomystory. (2012, February 11). How to change your ostomy bag [Video]. YouTube. https://www.youtube.com/watch?v=l9PYMfqNGm0
Provincial Health Services Authority. (n.d.). Patient handling videos [Videos]. http://learn.phsa.ca/phsa/patienthandling/
World Health Organization. (2014, July 2). WHO: SAVE LIVES – Clean your hands – No action today; no cure tomorrow [Video]. YouTube. https://youtu.be/kOKeFv5VvY4
Online Learning Tools
The following materials are ready for use in the classroom. A brief description and estimated time to complete each activity is included for each.
Provincial Infection Control Network of B.C. (2017). Infection prevention and control practices modules. https://www.picnet.ca/education/education-modules/infection-control-module/
- This online module covers the basics of infection control and hand hygiene in the health care system (60 minutes).
Social Care Institute for Excellence. (2014). Personal hygiene: Dignity in care [Video]. http://www.scie.org.uk/socialcaretv/video-player.asp?v=personal-hygiene
- A video with examples to illustrate how personal hygiene can be provided to clients using a person-centred approach to care (15 minutes).
WorkSafeBC. (2008). Assess every time [Video]. https://www.worksafebc.com/en/resources/health-safety/videos/assess-every-time?lang=en
- A video and discussion guide about the importance of assessment. (10–15 minutes).
WorkSafeBC. (2013). Ceiling lifts. Why aren’t they being used? [Video]. https://www.worksafebc.com/en/resources/health-safety/videos/ceiling-lifts
- A video and discussion guide about the use of ceiling lifts to reduce injuries (15 minutes)
WorkSafeBC. Home care visits. Find the hazards in this staged photo [Photo collection].
- A series of photos illustrating hazards that may be faced by health care assistants working in the home setting (30–60 minutes for review and discussion). Students can work together to identify what is wrong in each photo. Answers on reverse.
- (2015). Home care visits (outside the home). Closest to the home. https://www.worksafebc.com/en/resources/health-safety/posters/wwwtp-home-care-visits-outside-the-home/closest-to-home
- (2015). In the car [Photo]. https://www.worksafebc.com/en/resources/health-safety/posters/wwwtp-home-care-visits-outside-the-home/in-the-car
- (2015). Near the home. https://www.worksafebc.com/en/resources/health-safety/posters/wwwtp-home-care-visits-outside-the-home/near-the-home
- (2011). Slips and trips. https://www.worksafebc.com/en/resources/health-safety/posters/wwwtp-home-care-visits-inside-the-home/slips-and-trips?
- (2011). Soft tissue injuries. https://www.worksafebc.com/en/resources/health-safety/posters/wwwtp-home-care-visits-inside-the-home/soft-tissue-injuries?lang=en
- (2011). Violence, choking. https://www.worksafebc.com/en/resources/health-safety/posters/wwwtp-home-care-visits-inside-the-home/violence-choking
WorkSafeBC. (2008). Leave when it’s unsafe [Video]. https://www.worksafebc.com/en/resources/health-safety/videos/leave-when-its-unsafe
- A video and discussion guide describing what to do if you feel threatened or unsafe while working in the community setting (10–15 minutes for review and discussion).
WorkSafeBC. (2014). Make your home safer for care workers [Information sheet]. www.worksafebc.com/en/resources/health-safety/books-guides/make-your-home-safer-for-care-workers?lang=en
- An information sheet and checklist that can be used to discuss the safety of HCAs working in the home setting (10–15 minutes for review and discussion).
WorkSafeBC. (2009). Working with dementia: Safe work practices for caregivers [Videos]. https://www.worksafebc.com/en/forms-resources#q=Working%20with%20Dementia&sort=relevancy&f:content-type-facet=[Videos%20%26%20slide%20shows]&f:language-facet=[English]
- A series of six videos about working with dementia.
- Island Health. (2012). Changes have been made to the case scenarios and learning activities contained within the original source document (p. 87): Health Care Assistant Program Provincial Curriculum (2015) Supplement by the B.C. Ministry Of Advanced Education, licensed under a Creative Commons Attribution-ShareAlike 3.0 Unported License (CC BY-SA 3.0) ↵
- Island Health (2012). ↵
- A gait belt may also be called a walking, ambulation, or transfer belt, depending on the setting. HCA instructors may wish to lead a discussion about related equipment used by HCAs and other health care professionals in their local health authorities. ↵

