Main Body
CHAPTER 5: WHEN THE PROBLEM IS PAIN
Assessing for pain
Debra Dusome, R.N., Ex.A.T., M.A. (Psychiatric Nursing)
Introduction
Just like all people, individuals with intellectual disabilities experience pain. People with intellectual disabilities experience chronic pain related to medical conditions such as arthritis, cerebral palsy with significant spasticity, heart conditions, migraines, toothaches, earaches, infections, and other health issues. They experience pain related to traumatic injuries such as falls, accidents, broken bones, bruising, and injury from violence perpetrated against them. Some health condition interventions such as surgery or assessment procedures may be intrusive and painful. Medical assessments and treatment interventions can be scary and painful for any person, but they can be especially frightening for an individual with both intellectual disabilities and mental health challenges. Medical assessments and interventions often lead to an increase in anxiety, and sometimes aggressive behaviour, when individuals don’t understand what and why certain events are happening (McKenzie, Smith & Purcell, 2012).
According to McCaffrey (1968), pain is whatever the experiencing person says it is and exists whenever he or she says it does. But a problem arises when individuals cannot report what is happening to them. The majority of individuals with intellectual disabilities are able to give some account of the pain they are experiencing, but the descriptions of localization of the pain and the potential origins of the pain can be difficult for some to articulate (Findlay, Williams & Scior, 2014; Hennequin, Morin, & Feine, 2000). Individuals who lack expressive language and have limited comprehension of language can usually only articulate their distress through changes in behaviour and facial expression, so pain must be assessed using a combination of behavioural cues and proxy information (information provided by others) (Davies & Evans, 2001).
Ethical Principles for Addressing Physical Health Conditions and Assessing Pain
The ethical principles of beneficence (the duty to benefit another) and non-maleficence (the duty to do no harm) oblige health care professionals, caregivers, and direct support staff to provide medical care for health problems and pain management and comfort to all individuals, including those who are unable to speak for themselves (Herr et al., 2011). The principles of justice (the equal treatment of individuals) and respect for human dignity also require support workers to do the best for individuals in their care.
The Hierarchy of Pain Assessment Techniques
Pain assessment techniques should follow a logical progression or hierarchy such as the one devised by Herr and colleagues (2011).
Obtain self-report. Get as much self-report of pain as possible. This may be a simple yes or no head nod or vocalization. It could include pointing or hand grasps or eye blinking. If a self-report is not possible, state the reason and proceed with assessment.
Search for potential causes of pain. Does the individual have arthritis or other chronic medical conditions that could be causing pain? Has the person experienced a trauma that would cause pain or has he or she experienced surgery or treatments such as wound care, blood tests, rehabilitation activities, or positioning/turning that are normally known to cause pain? Does the person show a significant change in behaviour such as signs of trouble with breathing, fainting, or change in bowel movements or passing urine?
Observe the person’s behaviour. Use valid and reliable behavioural pain measurement tools. Look for a change in the individual’s normal behaviour patterns, such as a normally outgoing person becoming more withdrawn, or a quiet, passive person starting to strike out aggressively, or a person engaging in self-injurious behaviour that is not typical (Bosch, 2002; Carr & Owen-Deschryver, 2007). Sleep and apparent sedation do not necessarily rule out a person experiencing pain. It is important that the assessment for pain involves the caregiver or staff person with the greatest knowledge of the person and his or her regular behaviours.
Obtain proxy reports of pain and behaviour/activity changes. Credible information can be obtained by proxy (from family members, parents, unlicensed or professional caregivers) who know the individual well. Parents and consistent caregivers are often the best sources of reliable information to assist with pain assessment. These individuals may have direct knowledge of how the person has responded to painful or illness-related situations in the past. They may be able to pick up on subtle signs that a new caregiver may not notice. Combine proxy information with direct observation of the individual and a thorough health assessment and examination. Proxy information does not take the place of a thorough physical, mental, and diagnostic workup.
Attempt a trial of pain relief medication or comfort measures. If mild or moderate pain is suspected, try comfort measures and non-opioid (non-narcotic) medications such as acetaminophen or ibuprofen every six hours for 24 hours. If behaviour improves, assume pain was the cause. For severe pain, a low-dose short-acting pain reliever such as hydrocodone or morphine should be given as a one-time dose under the direction of a physician to see if it brings relief. If so, a routine of regular pain medication may be ordered to manage pain. If pain or distress is not relieved after a reasonable pain relief trial with medication, then further assessment is required to identify the potential problem. In individuals with intellectual disabilities it is important to start with a lower dose of medication and work up to an effective dose, as these individuals may have greater sensitivities to medications. Go slowly, but the ultimate goal is to treat the pain effectively.
 The Hierarchy of Pain Assessment Techniques
The Hierarchy of Pain Assessment Techniques
Key Points for Caregivers
Hierarchy of Pain Assessment
- Obtain self-report.
- Search for potential causes.
- Observe behaviours.
- Obtain proxy reporting.
- Attempt trial of pain medication.
Guiding Principles Pain Assessment
People with intellectual disabilities have been cognitively impaired since birth or early childhood, and their intellectual disability continues throughout their lifetime (Herr et al., 2011). Intellectual disabilities can be accompanied by physical disabilities as well (Bottos & Chambers, 2006). An IQ of 50 to 70 indicates mild cognitive impairment and represents 85% of the population of people with intellectual disabilities. The majority of these individuals are verbal and usually acquire academic skills to the level of Grade 6. Most can self-report on their pain and the circumstances related to their pain. Individuals with an IQ below 50 have moderate, severe, or profound cognitive impairments. The Faces Pain Scale—Revised (see figure 5.1) can be used for those with suspected mental age greater than five years of age (Goodenough et. al., 1999).
Bottos and Chambers (2006) report that both children and adults with intellectual disabilities have higher tolerance for pain experiences when compared with healthy individuals. This may be related to challenges in recognizing and communicating pain to others. People with intellectual disabilities have been observed carrying out normal daily activities even when they have been seriously injured. Children and adults with intellectual disabilities often have medical conditions that require ongoing treatment or regular procedures and investigations that are associated with pain. Caregivers, family members, and professional caregivers need to regularly assess for the presence of pain, its location, and its severity. Once pain is identified, it needs to be treated and comfort measures provided.
Individual behavioural responses to pain vary from an increase in activity, such as pacing and vocalizations, to dampening of behaviours, such as becoming quieter and isolating from others. Although there have been some reports of differing sensitivities to pain (Foley & McCutcheon, 2004), most children and adults with intellectual disabilities do have intact sensory function (Symons, Shinde, & Gilles, 2008), which means they feel pain. However, people with intellectual disabilities may not express pain in the ways others do, and therefore it is important for caregivers to understand an individual’s specific response to pain (Cheetham, 2001; Chivell, 2001; Temple et al., 2012; McGraft et al., 1998). Neurological perception and motor and/or communication abilities of an individual with intellectual disabilities can create challenges for others to effectively recognize that the individual is in pain. This can result in under- or overestimation of pain, which is why it is important to have people who know the individual well involved in the pain assessment and treatment process.
Behavioural Pain Assessment Tools
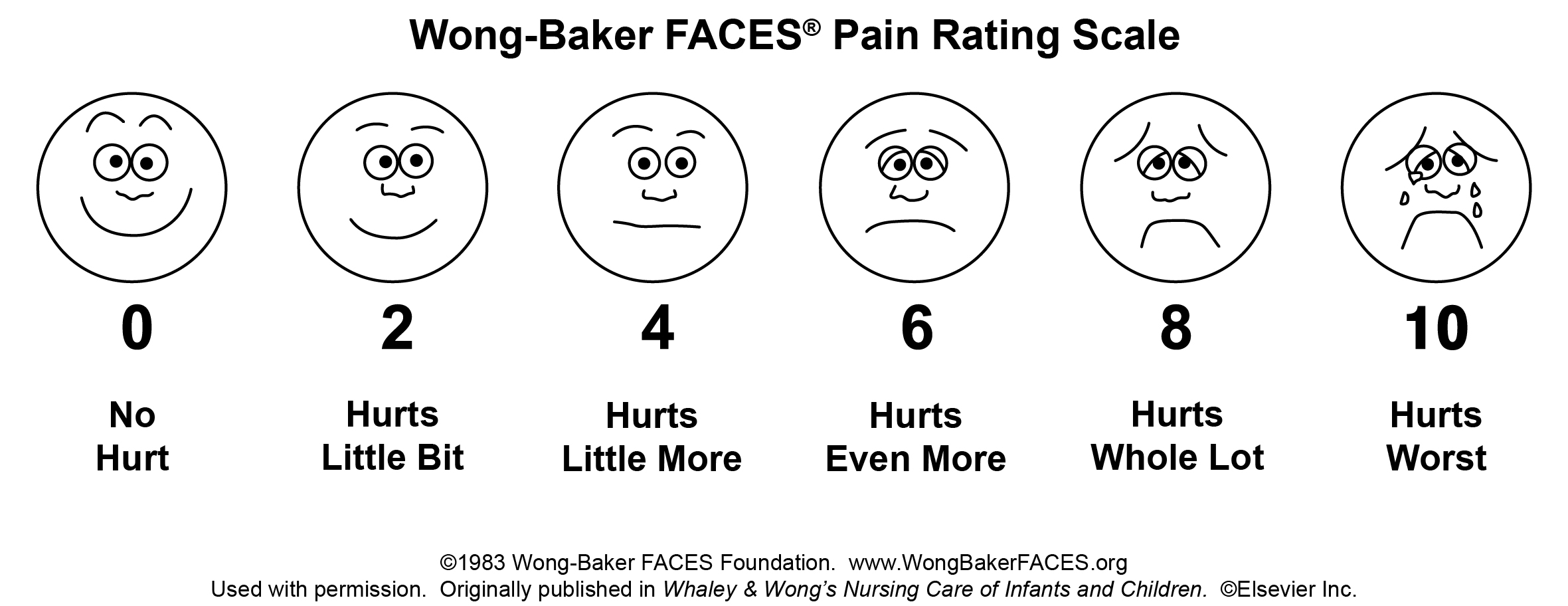
According to Keck and colleagues (1996), children and adults, including those with intellectual disabilities, can point to the face on a pain scale that indicates their pain level. Individuals who can count and understand numbers can use the number scale, and those who can read can successfully use the word scales. The individual needs to comprehend the relationship of the scale to his or her experience of pain. The picture faces are often preferred as pain indicators and have been found to be successfully used by people with moderate and severe cognitive disabilities. Identifying possible causes for the pain and developing a treatment plan for most individuals with severe and profound levels of disability will also require proxy information and a thorough physical assessment. Although the Faces Pain Scale can indicate the presence of pain, it cannot identify the cause or location of pain.
Individualized Numeric Rating Scale
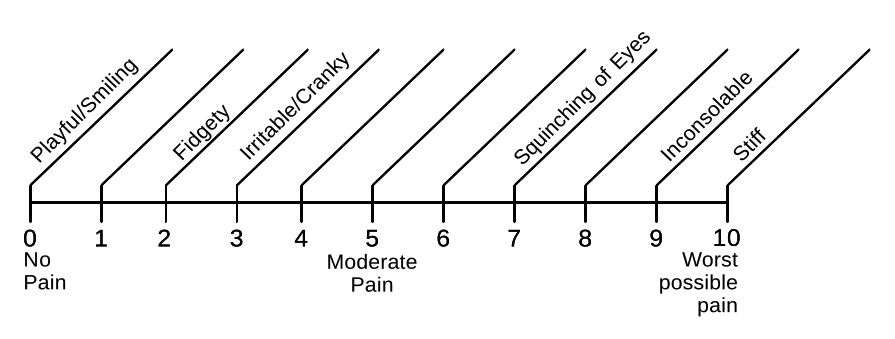
The Individualized Numeric Rating Scale (Curley, 2010) has primarily been used to assess pain in children with profound intellectual disability who are unable to use words to express pain (see the figure 5.2). These individuals depend on parents or caregivers who know them extremely well to report on their levels of pain. Several studies have demonstrated that parents of children with intellectual disabilities can describe their child’s pain indicators (Carter, McArthur, & Cunliffe, 2002; Hunt et al., 2003; Voepel-Lewis, Maliviya, & Tait, 2005).
Care must be taken when transferring the use of the Numeric Rating Scale to adults and to people who do not have a consistent relationship with the individual with severe and profound intellectual functioning. Ideally, the setting should have some sort of documented health history of the individual, whether that is an institution, group home, assisted living, with family members or foster caregivers, or independent with supports. If the parents of the individual are still living and have regular contact with their son or daughter, they can provide a health history and their child’s individual response to pain, health challenges, and visits to the doctor, dentist, and other health care providers. This information is valuable for helping the caregiver assess pain.
The Individualized Numeric Rating Scale is typically used in acute health care settings where the individual is receiving surgery, is in intensive care, or undergoing procedures known to be extremely painful, such as caring for severe burns. The parents or consistent caregiver are asked to fill in the scale with behavioural indicators of pain (Solodiuk et al., 2010). To do this they must have personal knowledge of the person when they are well and experiencing no pain. They must also have personal knowledge of behavioural indicators when the person has mild pain (headache, stomach ache), moderate pain (earache, toothache), or severe pain (broken bone, severe traumatic injury, post-surgery). The scale is then filled in with that person’s individual responses, such as rocking when in moderate pain, history of head punching when having experienced a previous punctured eardrum, etc. These behavioural indicators are then used to provide the optimal level of pain relief.
FLACC Pain Assessment Scale
The FLACC Pain Assessment Scale (Merkel et al., 1997) looks at five categories of behaviour in an individual: (F) face, (L) legs, (A) activity, (C) cry, and (C) consolability. Each of the five categories is scored from 0 to 2, which results in a total score between 0 and 10. The higher the score on this instrument, the higher the pain (see Table 5.1).
Table 5.1 FLACC Pain Assessment Scale
| Scoring | Scoring | Scoring | |
| Categories | 0 | 1 | 2 |
| (F) Face | No particular expression or smile | Occasional grimace or frown, withdrawn, uninterested | Frequent to constant frown, clenched jaw, quivering chin |
| (L) Legs | Normal position or relaxed | Uneasy, restless, tense | Kicking or legs drawn up |
| (A) Activity | Lying quietly, normal position, moves easily | Squirming, shifting back and forth, tense | Arched, rigid, or jerking |
| (C) Cry | No crying (awake or asleep) | Moans or whimpers, occasional complaint | Crying steadily, screams or sobs, frequent complaints |
| (C) Consolability | Content, relaxed | Reassured by occasional touching, hugging, or talking to, distractable | Difficult to console or comfort |
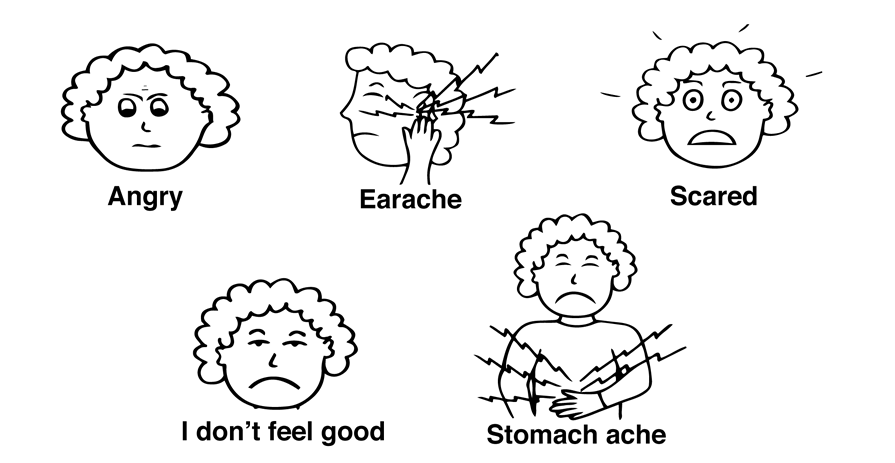
Picture Resources for Identifying Emotions of Physical Distress
For individuals who have functional language comprehension but limited expressive language, pictures can often be used to indicate wants, needs, or signs of distress. The website of Do2Learn Educational Resources for Special Needs (http://www.do2learn.com) includes many resources and programs for people working with individuals with special needs, including pictures that can be used for identifying emotions of physical distress. Pictures can be found at http://www.do2learn.com/picturecards/printcards/2inch/imagegrids.
The pictures shown in figure 5.3 are samples of some of the images that may be useful for working with individuals with intellectual disability. Copies could be made and laminated for use in household, group home, school, or work settings. Alternatively, a binder could be compiled for each individual, with images that are useful for that person’s communication with others.
Using the Disability Distress Tool
Meaningful communication with individuals with profound communication limitations depends on family members, caregivers, or support workers to identify and translate verbal, visual, or sound cues. Distress means many different things to different people (Regnard et al., 2007). Most people would agree that distress relates to more than just pain and physical discomfort. Many individuals with intellectual disabilities can give cues that they are distressed but may not be able to clearly communicate the source of their distress. This is most important for the individual who experiences cognitive, physical, and mental health challenges. Most distress cues are identified as deviations from the individual’s normal way of being in the world. For this reason, it is important to identify the characteristics of an individual when he or she is content, so that caregivers can identify a change in verbal, visual, and sound cues when the individual is in distress.
Regnard and colleagues (2007) emphasize that while distress may be hidden, it is never silent. People with intellectual disabilities have differing abilities for receiving, understanding, remembering, and expressing themselves through use of verbal and non-verbal language. They depend on others to recognize and translate their specific language of signs and behaviours. The Disability Distress Tool (DisDAT) was designed by Regnard and validated by his research team to help caregivers recognize and respond to distress in individuals with intellectual disabilities (see Table 5.2). When using the DisDAT, it is critically important to document signs and cues when an individual is content to compare with signs and cues he or she displays when distressed.
Table 5.2 DisDAT. Most common signs and behaviours (cues) presented by individuals with disabilities when content and when distressed
| Contented cues (signs and behaviours observed in person when content) | Percentage presenting with these cues | Distressed cues (signs and behaviours observed in person when distressed) | Percentage presenting with these cues |
| Smiles | 80 | Lifts hands to head | 50 |
| Vocalizes without prompting | 70 | Screams, wails | 40 |
| Has relaxed body/face | 50 | Withdraws | 40 |
| Laughs | 40 | Becomes quiet | 30 |
| Responds vocally to social interaction | 40 | Groans | 30 |
| Has bright eyes | 40 | Face is bright red | 30 |
| Makes eye contact | 40 | Body is rigid | 30 |
| Eyes move around | 30 | Looks tearful, sad | 20 |
| Gestures towards social partner (spontaneous and response) | 30 | Is restless | 20 |
| Is affectionate | 30 | Clenches and grinds teeth | 20 |
| Is quiet | 30 | Grimaces, face is distorted | 20 |
| Sits straight/upright | 20 | Body is slumped | 20 |
| Blows raspberries | 20 | Uses different tone in vocalization | 20 |
| Grimaces | 10 | Face is rigid | 10 |
| Grinds teeth | 10 | Curls into themselves | 10 |
| Head is upright | 10 | Is not smiling | 10 |
| Is involved in interactions and environment | 10 | Makes growling noises | 10 |
| Likes close proximity | 10 | Eyes widen | 10 |
| Makes sighs of contentment | 10 | Increases eye movement | 10 |
| Co-operates with interventions | 10 | Breathes shallowly | 10 |
| Taps feet to music | 10 | Has shortness of breath | 10 |
Both people who know the individuals and those who do not know them are able to identify distress using the DisDAT tool. However, people who know an individual’s specific signs and cues able to identify the distress earlier. (Distress is noted as a change from contented behaviours to behaviours that indicated distress.) Keep in mind that each person typically has his or her own language of distress. The DisDat is available online at http://prc.coh.org/PainNOA/Dis%20DAT_Tool.pdf
Pain and Health Care for Dually Diagnosed Persons
People with intellectual disabilities and mental illness deserve the same standard of care as all other individuals. This means they should have regular annual checkups with a physician, a dentist, and any other health professional who is regularly involved in their care, such as a physiotherapist or occupational therapist. Individuals may have one or more medical conditions that require more regular follow-up (for example, diabetes that requires monitoring by a physician every three months). Caregivers should expect and advocate for this level of care to ensure that complications related to disease processes are detected early. People with intellectual disabilities may require a longer appointment time and/or may feel more comfortable if a person they trust accompanies them to their appointments (see Chapter 4).
Unfortunately many people with dual diagnosis receive substandard care, perhaps because a health care professional holds prejudicial beliefs about individuals with intellectual disabilities, or simply because he or she does not know how to care for individuals with intellectual disabilities. If an individual has experienced diagnostic testing and surgical procedures in the past without adequate pain treatment, or didn’t understand what was happening or what was expected, he or she may be fearful and anxious before health care visits. Similarly, when health care services have not recognized, treated, or managed an individual’s pain well, the caregiver can leave the experience feeling the negative emotional impact (Findlay, Williams, Baum, Scior, 2014).
The gold standard for good pain assessment is to have the individual self-report symptoms as much as he or she is able before a proxy adds information. Caregivers should report regular behaviour, any changes that they have observed, and whether they have seen these responses in the past related to specific health care concerns.
None of this information takes the place of a thorough physical assessment and diagnostic workup by a health care professional. Ideally, clients should see health care professionals who know them well and who have the individual’s health care history. In emergencies and in situations where the individual is in obvious pain or distress, they may see health care professionals they have never met before. This can be quite frightening and anxiety-provoking for many individuals, especially for those who also have mental health issues (see Chapter 3). Thus, it is important that the individual be accompanied to appointments or to the emergency department by a family member or caregiver who knows the most about the person, who can provide comfort, and who is trusted by the person. Many people with intellectual disabilities may require some anxiety medication or sedation for complex dental or medical procedures, so they really appreciate having someone with them who cares. Often an individual can be helped by distracting activities, ongoing conversations, a comforting object, or a promise of an enjoyed activity after a health care visit.
Conclusion
In this chapter we have discussed the experience of pain. Health care providers, direct support workers, and all those who care for and about individuals living with intellectual disabilities have an ethical duty to implement pain assessments with both verbal and non-verbal information. Often the main indicators that a person is in distress are behavioural cues and information from others. The progression or hierarchy of steps to assess pain are 1) obtain a self-report, 2) search for potential causes, 3) observe behaviours, 4) obtain information from others (proxy reporting), and 5) attempt a trial of pain medication. People may experience pain even when they are carrying out normal daily activities, and therefore a guiding principle is to involve those who know the person throughout the process of assessing and treating pain.
Five tools to assess physical pain have been explained: 1) the Wong-Baker FACES® Pain Rating Scale, 2) the Individualized Numeric Rating Scale, 3) the FLACC Pain Assessment Scale, 4) pictures for identifying distress, and 5) the DisDat. We have emphasized how dually diagnosed people require regular checkups that include thorough physical assessments and diagnostic workups. During complex medical procedures, caregivers can request that health care professionals provide anxiety medications. Caregivers can provide distracting activities or an enjoyable activity after the procedure. Assessing and responding when dually diagnosed people say or show that they are in pain is a critical element in supporting them toward living healthy lives.
Chapter Audio for Print
 This chapter contains a number of short audio clips. If you are reading this in print, you can access the audio clips in this chapter by scanning this QR code with your mobile device. Alternatively, you can visit the book website at opentextbc.ca/caregivers and listen to all the audio clips.
This chapter contains a number of short audio clips. If you are reading this in print, you can access the audio clips in this chapter by scanning this QR code with your mobile device. Alternatively, you can visit the book website at opentextbc.ca/caregivers and listen to all the audio clips.
References
Bosch, J. J. (2002). Use of directed history and behavioural indicators in the assessment of the child with a developmental disability. Journal of Pediatric Health Care, 16(40), 170–179.
Bottos, S. & Chambers, C.T. (2006). The epidemiology of pain in developmental disabilities. In T. F. Oberlander, & E. J. Symons (Eds.), Pain in children and adults with developmental disabilities. Baltimore MD: Brookes.
Carr, E.G. & Owen-Deschryver, J. S. (2007). Physical illness, pain, and problem behaviour in minimally verbal people with developmental disabilities. Journal of Autism and Developmental Disorders, 37(3), 413–424.
Carter, B., McArthur, E., & Cunliffe, M. (2002). Dealing with uncertainty: parental assessment of pain in their children with profound special needs. Journal of Advanced Nursing, 38 (5), 449–457.
Charleston Pediatric Pain Pictures (n.d.). Retrieved from the Charleston Pediatric Dentistry website at http://www.google.ca/search?q=charleston+pediatric+pictures
Cheetham, T. C. (2001). Challenges in medical care for persons with developmental disabilities: An illustrative case “RAR”. Clinical Bulletin of the Developmental Disabilities Program, 12, 1–9. Retrieved from http://www.psychiatry.med.uwo.ca/ddp/bulletins/01sepbul.htm.
Chivell, W.C. (2001). An inquest taken on behalf of our Sovereign lady the Queen at Adelaide in the State of South Australia, on the 2nd and 3rd and 17th of July 2001 and the 24th of August 2001, before Wayne Cromwell Chivell, a Coroner for the said State, concerning the death of Saverio Gadaleta. Adelaide, Coroners court, South Australia, pp. 1–10.
Curley, M. A. (2010). The Individualized Numeric rating Scale (INRS). Image and instructions for use. Retrieved from www.marthaagcurley.com/inrs.html
Davies, D. & Evans, L. (2001). Assessing pain in people with profound learning disabilities. British Journal of Nursing, 10 (8), 513–516.
Findlay, L., Williams, L., & Scior, K. (2014). Exploring experiences and understandings of pain in adults with intellectual disabilities. Journal of Intellectual Disability Research. 58, part 4, 358–367. doi: 10.1111/jir.12020
Findlay, L., Williams, A., Baum, S., & Scior, K. (2014). Caregiver experiences of supporting adults with intellectual disabilities in pain. Journal of Applied Research in Intellectual Disabilities, Jun 9 Epub. doi: 10.1111/jar.12109
Foley, D. C. & McCutcheon, H. (2004). Detecting pain in people with an intellectual disability. Accident and Emergency Nursing. 12(4), 196–200.
Goodenough, B., van Dongen, K., Brouwer, N., & Abu-Saad, H. (1999). Champion GD: A comparison of the Faces Pain Scale and the Facial Affective Scale for children’s estimates of the intensity and unpleasantness of needle pain during blood sampling. European Journal of Pain, 3(4), 301–315.
Hennequin, M., Morin, C., & Feine, J. S. (2000). Pain expression and stimulus localization in individuals with Down’s syndrome. Lancet 356 (9245), 1882–1887.
Herr, K., Coyne, P., McCaffery, M., Manworren, R., & Merkel, S. (2011). Pain Assessment in the Patient Unable to Self-Report: Position Statement with Clinical Practice Recommendations. Pain Management Nursing, 12(4), 230–250.
Hunt, A., Mastroyannopoulou, K., Goldman, A., & Seers, K. (2003). Not knowing – the problem of pain in children with severe neurological impairment. International Journal of Nursing Studies 40, 171–183.
Keck, J., Gerkensmeyer, J., Joyce, B., & Schade, J. (1996). Reliability and validity of the Faces and Word Descriptor Scales to Measure Procedural Pain. Journal of Pediatric Nursing, 11(6), 368–374.
McCaffery, M. (1968). Nursing practice theories related to cognition, bodily pain, and man-environment interactions. Los Angeles CA: University of California at Los Angeles.
McGrath, P. J., Rosmus, C., Camfield, C., Campbell, M. A., & Hennigar, A.W. (1998). Behaviours caregivers use to determine pain in non-verbal, cognitively impaired individuals. Developmental. Medicine and Child Neurology. 40 (5), 340–343.
McKenzie, K., Smith, M., & Purcell, A. (2012). The reported expression of pain and distress by people with intellectual disability. Journal of Clinical Nursing, 22, 1833–1842, doi: 10.1111/j.1365-2702.2012.04269.x
Merkel, S. J., Voepel-Lewis, T., Shayevitz, J. R., & Malviya, S. (1997). The FLACC: A behavioural scale for scoring postoperative pain in young children. Pediatric Nursing 23, 293–297.
Regnard, C., Reynolds, J., Watson, B., Matthews, D., Gibson, L. & Clarke, C. (2007). Understanding distress in people with severe communication difficulties: developing and assessing the Disability Assessment Tool (DisDAT). Journal of intellectual Disability Research, 51, Part 4, 277–292.
Solodiuk, J. C., Scott-Sutherland, J., Meyers, M. et al. (2010). Validation of the Individualized Numeric Rating Scale (INRS): A pain assessment tool for non-verbal children with intellectual disability. Pain, 150(2), 231–236. doi:10.1016/j.pain.2010.03.016.
Symons, F. J., Shinde, S. K., & Gilles, E. (2008). Perspectives on pain and intellectual disability. Journal of Intellectual Disability Research, 52 Part 4, 275–286.
Temple, B., Dubé, C., McMillan, D., et al. (2012). Pain in people with developmental disabilities: A scoping review. Journal on Developmental Disabilities, 18 (1), 73–86.
Voepal-Lewis, T., Malviya, S., & Tait, A. R. (2005). Validity of parent ratings as proxy measures of pain in children with cognitive impairment. Pain Management Nursing 6 (4), 168–174.
Wong-Baker FACES Foundation. (2015). Wong-Baker FACES® Pain Rating Scale. Retrieved with permission from http://www.WongBakerFACES.org

