Cognitive and/or Mental Health Challenges
Download student handouts: Cognitive and/or Mental Health Challenges handouts [Word doc].
Course Guideline
The main focus of this course (at least 70%) should be on:
- Learning Outcome 1: Describe ways to organize, provide, and evaluate person-centred care and assistance for clients experiencing cognitive challenges.
- Learning Outcome 3: Describe effective approaches to responding to responsive and reactive behaviours.
A maximum of 30% of course hours should be dedicated to:
- Learning Outcome 2: Describe ways to organize, provide, and evaluate person-centred care and assistance for clients experiencing mental health challenges.
Suggested Learning Strategies
Strategies that Focus on Caring
1. Contributing to a Broadened Understanding of Cognitive Challenges
Invite students to imagine what it is like to suffer from a cognitive challenge, particularly dementia. Have students sit comfortably, close their eyes, and take several deep breaths.
Speaking softly, lead students through the following scenario:
Imagine yourself walking alone through a forest. It’s a lovely warm spring day. The sights, sounds, and smells of the forest are refreshing, and you are enjoying your walk.
As the afternoon progresses, you realize you aren’t sure which direction you should take to get back to your friends and family. As you look around, you realize that you are lost.
As you realize your situation, you experience a twinge of fear. You decide to keep walking in hopes of seeing something familiar, but find that the further you go, the more lost you become. Time passes and your fear verges on panic. As evening draws closer, you realize that you may have to spend the night alone in the forest.
Invite students at this point to open their eyes and discuss their bodily experiences, feelings, and thoughts. Invite them to discuss how this is similar to what some individuals with cognitive challenges might experience.
The client with cognitive changes may constantly feel lost. No matter what they do or where they go, they can find nothing that is familiar. What feelings would this person be likely to have? How is this related to some of the behaviours we might see in a person with cognitive challenges?
Invite students to close their eyes once again and visualize themselves back in the forest. Continue the scenario as follows:
You are back in the forest, still feeling lost and fearful. As dusk begins to settle, you notice that there is a strange person who seems to be following or observing you.
Can you see them? They are about 9 metres (30 feet) away. When you attempt to speak to this person, they answer in a language you don’t understand.
Invite students to open their eyes and describe their responses to the stranger. Some questions to encourage discussion:
- What feelings were stimulated?
- How does this relate to how individuals with cognitive challenges might experience the people in their environment (even family members)?
- How might this help us understand some of their responses?
Note: Some students may feel distressed by this activity. A content or trigger warning may be helpful. The following resource provides guidance on how to create a content or trigger warning.
University of Connecticut. (2024). Trigger and content warning guidance. https://provost.uconn.edu/trigger-warning/
2. Contributing to Person-Centred Care
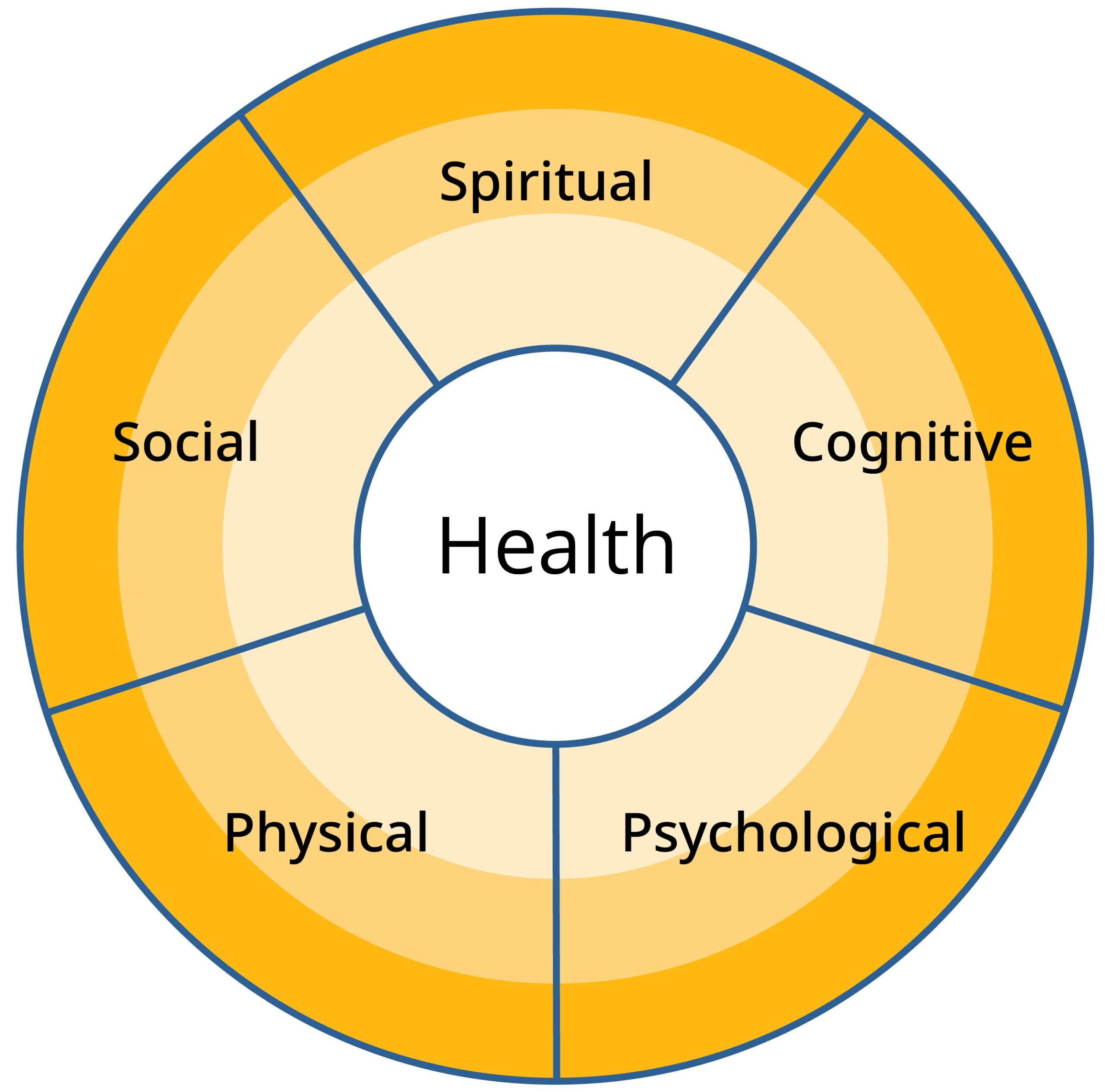
- Using the health wheel below as a guide, invite students to work in small groups to discuss how cognitive challenges might affect all areas of the dimensions of health: physical, psychological, cognitive, social, and spiritual. Then ask the groups to discuss how changes in each dimension of health might positively contribute to improved quality of life for the affected individual. Invite each group to report back to the whole class. An alternative to this activity is to provide students with scenarios of real or fictitious individuals who are experiencing a cognitive challenge. Ask students to focus their small group discussions on a specific scenario.
- Another alternative to this activity is to use scenarios that focus on family members (e.g., wife, husband, partner, daughter, son) who are supporting a person with a cognitive challenge. This time ask students to discuss in small groups how an individual’s cognitive and perceptual changes affect a family member. Students should consider all dimensions of the health wheel. Discussion should also focus on how this understanding might influence caregiver practice. Invite each group to report back to the whole class.
Note: The health wheel is first introduced in Lifestyle and Choices. See this course for more information.
3. Unfolding Case Study: Caring for Peter Schultz
As a homework assignment, ask students to review relevant textbooks, online courses, or other course materials related to communicating with clients with dementia.
Whole Class or Small Group Activity
In class, briefly review the challenges to communication experienced by clients with dementia. Following this, create a table with three columns on the whiteboard or use the STUDENT HANDOUT 1 below.
- Column 1: Communication challenges. To provide a meaningful context for this activity, list the communication challenges experienced by Peter Schultz.
- Column 2: Impact on client and family. For each challenge listed, ask the students to consider and list the potential impact on the client and his family.
- Column 3: HCA strategies: Have students list communication strategies that an HCA could use to address the challenge and reduce the potential impact.
Note: You may wish to complete a few full examples through each of the columns and then ask the students to complete the remaining items in a small group. Throughout the activity and during the debrief, highlight further communication challenges and strategies not listed.
STUDENT HANDOUT 1
Communication Challenges and Impact: Supporting Clients with Dementia
| Communication Challenges for Peter Schultz | Impact on the Client and/or Family | HCA Strategies |
|---|---|---|
| Difficulty initiating or following conversation | ||
| Difficulty following instructions or rules related to a game or activity | ||
| Difficulty understanding written material or communicating in writing | ||
| Expressing confusion and/or the inability to understand what is being said | ||
| Expressing resistance when directed to complete tasks related to personal care and hygiene | ||
| Expressing anger and frustration related to the loss of ability to complete formerly known or routine activities (e.g., household repairs and maintenance) |
Metzger, Z. B. (2010). The Last Lap of the Long Run, Addendum to “On the Long Run”: An Account of our Travels with Dementia. This material is licensed under a CC BY-SA 4.0 licence.
4. Ambiguous Loss and Grief Discussion Activity
Using the Alzheimer Society’s resource Supporting clients through ambiguous loss and grief: Strategies for health-care providers as a reference, introduce the concept of ambiguous loss and grief to the class.
Explain that this resource is intended to help health care providers gain a better understanding of how loss and grief affect people with dementia and their family caregivers. It provides useful strategies to assist families with their multiple losses and grief and to help caregivers stay connected with the person with dementia while building strength and resilience as the disease progresses.
Using the INSTRUCTOR DISCUSSION GUIDE 1 below, explore the following questions with the students:
- What is ambiguous loss and grief?
- Why is ambiguous loss and grief different from other types of grief?
- How can HCAs provide support to individuals and families experiencing ambiguous loss and grief?
Invite students to share their response to the questions listed above. As ideas are forthcoming, write them on the whiteboard or flip chart. Use the instructor discussion guide to highlight any items they haven’t considered.
Note: To promote discussion, you could prepare a few copies of the resource Supporting clients through ambiguous loss and grief: Strategies for health-care providers to share with the class. You could also ask students to review the document as a homework assignment before the class discussion. To support a professional approach to practice, students could be provided with a link to the document for reference during their clinical placement and after completion of the program.
Copyright © Alzheimer Society of B.C. (2017). This is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License (CC BY-SA 4.0).
INSTRUCTOR DSCUSSION GUIDE 1
Ambiguous Loss and Grief
What is ambiguous loss and grief?
- Ambiguous loss is a type of loss that happens when a person with dementia is physically present but is experiencing changed cognitive abilities.
- A family member caring for a person with dementia may experience ongoing stress and grief due to the ambiguous loss of having their partner, spouse or parent still here, but not present in the same way as before.
Why is ambiguous loss and grief different from other types of grief?
- When a person is bereaved, they are likely to receive support from family and friends, and may eventually find closure through the natural grieving process.
- Ambiguous loss complicates grief. It’s often hard for a caregiver to know whether or how to grieve.
- Many aspects of the person with dementia are lost, but some remain. Family and friends may not recognize the caregiver’s need to grieve the many losses at different stages of the disease and receive support while the person with dementia is alive.
- The caregiver may feel like he or she is living in limbo, unable to fully grieve or resolve the losses that have already occurred while anticipating other losses that lie ahead.
How can HCAs provide support to individuals and families experiencing ambiguous loss and grief?
- Be sensitive to a wide range of caregiver grief reactions, including sadness, anger, anxiety, ambivalence, guilt, denial, and helplessness.
- Use empathetic listening skills.
- Validate the person’s feelings and experience in a non-judgmental way.
- Acknowledge and affirm caregivers’ strengths, success, and resilience in coping with losses and adapting to changes.
- Help families and individuals recognize and understand the feelings of ambiguous loss and work through them with the help of Alzheimer Society staff or other health care providers.
- Provide strategies to help caregivers learn how to live with ambiguous loss, and remain healthy and resilient.
- Help caregivers find creative ways to engage with the person with dementia.
- Make a referral to the Alzheimer Society of B.C.
- Encourage caregivers to practise good self-care, for example by staying socially and physically active, eating well, and engaging in the spiritual or religious practices that are important to them.
5. Trauma-Informed Practice: Discussion and Self-Reflection Journal Activity
Introduce the activity by explaining that students will review a case scenario designed to explore the intersection between trauma-informed practice, mental health, and cultural safety and sensitivity.
In small groups, have students work through the discussion questions on the STUDENT HANDOUT 2. After the small group discussion, ask students to submit a self-reflection journal entry about the scenario and what they discussed.
STUDENT HANDOUT 2
Trauma-Informed Practice: Discussion and Self-Reflection Journal
DIRECTIONS: Read the scenario and discussion questions below. First discuss the questions in your small group before answering the self-reflection journal questions.
Emma is an 80-year-old Indigenous woman from a community in Northern B.C. She was a prominent community worker, dedicating her time to local youth programs. Emma now receives home support services from an HCA to assist with bathing, dressing, and mobility. Over the past year, Emma has been experiencing symptoms indicative of depression, including prolonged periods of sadness, a noticeable decrease in energy, and difficulty concentrating.
In Emma’s community, mental health issues are often enveloped in silence, partly due to historical trauma and distrust toward the mainstream health care system, which has a legacy of mistreatment of Indigenous people. There is also a significant stigma associated with admitting to mental health struggles, often perceived as a personal failing rather than a health issue that requires professional intervention.
For these reasons, Emma faces the challenge of a community-wide reluctance to discuss mental health openly, influenced by past and ongoing experiences of marginalization and cultural disconnection. This environment has contributed to her reluctance to seek help, fearing judgment and misunderstanding from her community and health care providers.
Small Group Discussion Questions
Trauma-informed practice
- What historical events contributed to the trauma experienced by Indigenous peoples in Canada?
- How has this history of trauma impacted the mental health of individuals and their communities?
- What would be the characteristics of a trauma-informed approach in this scenario?
Cultural competency
- What actions can HCAs take to ensure their practice is culturally safe, sensitive, and respectful of the historical contexts that affect the health and well-being of Indigenous people in Canada?
- What is the connection between a trauma-informed approach and cultural competency in providing care to individuals with mental health challenges?
Access to mental health services
- Through a trauma-informed approach to care, identify and discuss the barriers and concerns that Emma faces as an Indigenous person who is attempting to access mental health care.
- What changes to the system do you feel could benefit and improve access to mental health services for Indigenous communities?
Self-Reflection Journal Questions
Think about your perception of trauma and mental health challenges before starting the HCA Program.
- How has your understanding of trauma and its impact on mental health changed?
- How will an understanding of historical trauma faced by Indigenous people change the way you provide care?
Strategies that Focus on Critical Thinking, Problem-Solving, and Decision-Making
1. Classroom Debate Activity
Invite students to engage in a debate about a topic discussed in this course (see debate topics below). Divide the class into small groups of three to five students and assign two groups to each of the topics outlined for a debate; one group will take a pros position toward the topic and the other group will take a cons position.
Ask each group to identify two to three reasons to support the position they have been assigned. Then, with the instructor acting as the moderator, the two groups will engage in a debate using the following structure:
- Each group provides a brief introduction to their position on the topic.
- In alternating format, the two groups present the two or three reasons identified to support their position.
- Each group provides a brief closing statement.
After the debate, briefly come together as a larger group and summarize the positions presented. Invite feedback from the students not involved in the debate and discuss other considerations. Alternate groups until all students have participated in a debate.
Debate topics for caring for individuals experiencing cognitive and/or mental health challenges:
- For clients with dementia, reality orientation is more effective than validation therapy.
- Is it ethical for HCAs to lie to clients when they are using validation therapy?
- A client demonstrating responsive behaviours should be moved from a communal setting to a quiet room.
- HCAs should support and assist clients with dementia who are in romantic or sexual relationships. (See LearningHub learning resources for more information about the course Supporting Sexual Health and Intimacy in LTC, Assisted Living, Group Homes, and Supported Housing).
- When a client with mild cognitive impairment makes decisions that their family doesn’t agree with, the HCA should always advocate for the client.
2. Supporting Clients with Dementia Scenarios
As a homework assignment, have students read relevant course or online materials describing challenges that may be experienced by people with dementia and their families and the role of the HCA in responding with appropriate care and support.
- Whole Class Reading and Discussion
- Using the STUDENT HANDOUT 3 below, read one of the following scenarios and use it as an example. Then have the students identify key information and observations from the scenario and list it in the first column. Following this, have students identify important considerations that could provide context for the scenario and list them in the second column. Lead the students in a discussion about how they, as HCAs, would respond to the scenario. (An INSTRUCTOR DISCUSSION GUIDE 2 on supporting clients with dementia has been provided below).
- Small Group Activity
- Divide the class into small groups, assigning each group one of the remaining scenarios. Using the student handout provided below, students should identify key information and considerations. The students should then identify how they, as HCAs, could respond to the same situation.
- Whole Class Activity Debrief
- Come back together as a class and have each group report on the key information, considerations, and potential responses identified. Use the INSTRUCTOR DISCUSSION GUIDE 2 to highlight any that were not identified.
STUDENT HANDOUT 3
Scenarios: Supporting Clients with Dementia
DIRECTIONS: Identify key information and observations from the scenario and list in the first column. Next, identify important considerations that could provide context for the situation and list them in the second column. Finally, consider how to best respond to the situation.
Example, Scenario 1
It is 1:00 p.m. – time for Jean’s scheduled bath. Although she willingly goes to the bathing room with her regular HCA, she pulls away and cries out when the HCA starts to remove her clothing. She becomes extremely agitated and the HCA is unable to calm her and continue with the bathing process. For the third week in a row, Jean returns to her room without bathing.
| Key Information | Considerations | HCA Responses |
|---|---|---|
|
|
|
Scenario 2
Maria usually goes to bed around 8:00 p.m. but always gets up at 2:00 a.m. and wanders the halls. When staff take her back to bed, she gets up again, saying she must take care of the baby.
| Key Information | Considerations | HCA Responses |
|---|---|---|
Scenario 3
Fiona has lived at a care home for the past two years. She has Alzheimer’s disease and now requires full assistance with personal care and dressing. She used to be a very classy dresser – everything matching, makeup always impeccable. Her daughter, Marjorie, is having a hard time adjusting to her mother’s changing abilities.
Today the HCA, Wenona, came in to help Fiona get ready for the day and Fiona was already dressed. Wenona noticed that the buttons of her blouse were done up incorrectly and her clothing neither matched nor clean. She also noticed that Fiona had brushed her hair but left a large piece sticking up at the back. Wenona was thrilled that Fiona had dressed and groomed independently and rather than correcting her errors, she chose to leave Fiona’s hair and clothing as they were, saying, “Fiona, you look nice today. I like the blouse you’ve chosen!” Later in the day when Marjorie visited, she was furious that staff had not “corrected” her mother’s outfit and hair.
| Key Information | Considerations | HCA Responses |
|---|---|---|
Scenario 4
Albert is a newly graduated HCA. He feels lucky to have secured full-time employment at a new complex care facility. During his HCA program, Albert took pride in taking the time to apply a person-centred approach with each of the clients he supported.
Despite his training and a sincere desire to help, he quickly feels discouraged and overwhelmed by the large workload and the attitudes of his colleagues, who Albert considers to be too task-focused. He does not feel that he can use anything he learned, since every minute of his day is spent racing through a series of tasks.
| Key Information | Considerations | HCA Responses |
|---|---|---|
Copyright © 2017, Alzheimer Society of B.C. This material is licensed under a CC BY-SA 4.0 licence.
INSTRUCTOR DISCUSSION GUIDE 2:
Supporting Clients with Dementia
| Key Information | Considerations and Potential Responses |
|---|---|
Scenario 1
|
|
Scenario 2
|
|
Scenario 3
|
|
Scenario 4
|
|
Copyright © 2017, Alzheimer Society of B.C. This material is licensed under a CC BY-SA 4.0 licence.
3. Person-Centred Care in Practice Scenario
Explore the role of the HCA in providing person-centred care to clients with dementia.
- Whole Class Review and Discussion
- Ask the students to respond to one or more of the following questions:
- What is person-centred care?
- How can health care staff provide person-centred care for clients with dementia?
- What does it mean to understand the reality of someone with dementia?
- Is it possible to provide person-centred care if you don’t know anything about dementia and how it progresses?
- How can you involve family?
- How can you provide choices to the person who appears unable to choose, and why is this important?
- How would you respond to the following statement: “Come on, sweetie. Let me help you get dressed”?
- As ideas are forthcoming, write them on the whiteboard or flip chart. Use the INSTRUCTOR DISCUSSION GUIDE 3 below on person-centred care in practice to highlight any items that were not considered. Discuss terms commonly used to address clients (e.g., love, dearie, etc.) and discuss why they are not appropriate. Ask students to identify appropriate ways to address clients (considering a client’s preference, culture, formality, etc.).
- Ask the students to respond to one or more of the following questions:
- Small Group Activity
- Divide the class into small groups. Ask the students to read the scenario on the STUDENT HANDOUT 4 below and respond to the discussion questions provided. To support completion of the small group activity, ensure that students can link to the reference document or provide printed copies.
- Whole Class Activity Debrief
- Briefly come back together as a group and have each group report on their responses. Use the INSTRUCTOR DISCUSSION GUIDE 3 below to highlight any considerations that were not identified.
*Copyright © Alzheimer Society of B.C. (2017). This material is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License (CC BY-SA 4.0).
STUDENT HANDOUT 4
Scenario: Person-Centred Care in Practice
DIRECTIONS: Read the scenario and respond to discussion questions provided.
Mr. Peterson has moderate dementia and has particular difficulty with his language. He never participates in any of the activities that the facility organizes. Today he walked over to the activity room and sat down at a table by himself. The recreation therapist, Dawn, asked one of the HCAs to take him back to his room. “He never participates anyway, so he probably just got lost,” she tells the HCA.
Small Group Discussion Questions
- Is this a person-centred response? Why or why not?
- How could the HCA respond to Dawn’s statement and the situation?
- If Dawn or the HCA were to involve Mr. Peterson in the activity, what should they consider?
- Why is meaningful activity critical to a person-centred approach?
- How could the HCA provide opportunity for meaningful activity while assisting Mr. Peterson with his activities of daily living (e.g., during the morning care routine)?
- How can you provide choices to the person who appears unable to choose? Why is it important to provide choices?
Copyright © 2017, Alzheimer Society of B.C. This material is licensed under a CC BY-SA 4.0 licence.
INSTRUCTOR DISCUSSION GUIDE 3
Person-Centred Care in Practice
Person-centred care
- Focuses on the individual, rather than the condition
- Focuses on the person’s strengths and abilities, rather than their losses
- Recognizes that the personality of the person with dementia is not lost, just increasingly changed by the disease
How can HCAs provide person-centred care for people with dementia?
- Focus on people with dementia as individuals – understanding the person’s history, values, likes, and dislikes
- Try to understand each person’s reality
- Remember that all behaviour has meaning
- Master effective and meaningful communication
- Recognize every person’s potential to engage socially and spiritually
- Talk to and about the person with dignified, non-judgmental and respectful language
- Provide choices, taking the person’s wishes into consideration, and obtaining consent, if possible
- Recognize feelings and provide support
- Demonstrate empathy
- Involve and support family and friends
- Focus on bringing out the best in the person and helping them to have a good day
- Bring these values into the last stages of dementia and the end of life
What does it mean to understand another person’s reality?
- Remember that a person’s reality does not have to be objectively real to be their reality.
- It is not helpful to try to “set the person straight” about what is really happening.
- Sometimes understanding the world from the perspective of the person with dementia means not only speaking to them but also to family and friends and being attentive to non-verbal cues. It helps to have a sense of where a person’s memory is at any given time. Putting their reality into a context of time and place can help you understand their reality; for example, if a person is talking or acting like they are in their 30s, it might make sense that they are talking about having a young daughter.
How can you involve and support a client’s family and friends?
- First and foremost, the staff needs to recognize what a move to complex care might represent for a family or care partner.
- HCAs should recognize that grief is a constant companion for families who are on the dementia journey.
- Families are valuable members of the care team.
- Families provide a sense of continuity for the person with dementia and can familiarize staff with the person’s likes and dislikes, values, wishes, and personality.
- A collaborative relationship with families benefits the person with dementia, their family members, and the staff of the care home.
- Some families will be very difficult, for a variety of reasons. A referral to counselling or the Alzheimer Society of B.C. might be the best choice under such circumstances.
“Come on, sweetie. Let me help you get dressed.” Is there anything wrong with this statement?
- Ask yourself if referring to someone under your care as “sweetie” is dignified and respectful.
- Do you talk to your parents that way?
- Most care staff would say that using endearments like “sweetie,” “dear,” “honey,” or “mama” is not done with bad intentions. They want to be nurturing, which is a commendable intention. But these terms are likely not appropriate under the circumstances.
- What are other ways that you can be nurturing, yet respectful of the person’s dignity?
Would you say Dawn is providing person-centred care? Please explain why you answered the way you did.
- This is not person-centred care.
- Dawn does not speak to Mr. Peterson; she talks about him to the HCA, as if he was not there.
- Just because he hasn’t participated in the past does not mean that he can’t change his mind and decide to participate today. Dawn is disregarding Mr. Peterson’s potential to engage socially.
How can you provide choices to the person who appears unable to choose? Why is this important?
- Choice is a key component of personal agency; we are able to make choices for ourselves as adults. Removing any sense of choice from the person with dementia robs them of their independence.
- You can incorporate the values, beliefs, cultural, and spiritual backgrounds of people with dementia and their families into the planning and delivery of care.
- You can recognize that dementia does not diminish a person. Rather, it changes the person’s capacity to interact with their environment.
- As dementia progresses and it becomes increasingly difficult to obtain fully informed consent from people with dementia, it is still possible to involve them in the decision-making process to some extent. Keep them informed and find out from their family, representative, or temporary decision-maker what their preferences are.
- Respect dissent. This is often expressed through behaviour, like turning their head away, biting, pushing or walking away.
- Frame your words and actions in “choice” language, so even if you really are only offering one choice, it still appears to be a choice and not an imposition.
4. Mental Health Resource Collaboration
Have students research, vet, and share mental health information and resources collectively as a class.
These resources could include personal mental health supportive apps that can be downloaded onto smartphones, community support programs, information from health authorities, and provincial or federal websites with information regarding mental health. The resources can also vary in their core purpose. For example, they could be resources that primarily provide information about mental health and mental health challenges or resources that provide students with daily activities or health services that support their mental health. The activity could be ungraded or graded based on participation (for example, each student could be asked to find two resources).
Invite students to share resources in person or online. Students could post resources on a physical bulletin board in the classroom, or they could post the resources to an online imageboard or forum. Instructors should investigate the available applications within the learning management systems provided by their institution before investigating external software that may require payment.
Strategies that Focus on Professional Approaches to Practice
1. Mental Health Challenges Discussion
- Self-Reflection
Invite students to reflect individually on the following questions. This could be done through a journal activity prior to the small group in class discussion. As the content of the students’ reflections may be sensitive and include personal or familial trauma, instructors may want to have students complete this journal without requiring them to submit it to respect students’ privacy.- What are your concerns or fears about people experiencing mental health challenges? What has caused you to have these concerns?
- Do you have any friends or family members who have had experiences with mental health challenges? If so, how has this influenced your feelings about mental health?
- Do you think you would enjoy working with individuals with mental health challenges? On what do you base your response to this question?
- Small Group Discussion
Invite students to form small groups to discuss the following:- How is the caregiver role, whether in the community or a facility, different when the client is experiencing a mental health challenge as opposed to a physical health challenge?
- What personal and professional caregiver characteristics would be most valuable when working with individuals with mental health challenges? Encourage them to consider characteristics related to:
- Personality/temperament
- Knowledge about mental health
- Ability to form relationships with clients
- Need for control
- Ability to work with other health care team members
- Ability to interact with family members
- Other characteristics that seem important
- What legal and ethical issues are particularly important to be aware of when working with clients experiencing mental health challenges?
2. Diverse Perceptions of Mental Health Challenges: Self-Reflection Journal
Introduce the activity by explaining that perceptions of mental health and mental health challenges may differ between diverse groups. Diverse factors such as cultural background, religion/spirituality, generation, socio-economic status, gender, and personal experience can affect how people perceive mental health challenges in themselves and others.
Clarify with students that the purpose of the activity is to reflect on their own perceptions about mental health, the factors or experiences that have influenced those perceptions, and how their perceptions and experiences might influence the care they provide to clients experiencing mental health challenges.
Show the video:
TEDx Talks. (2015). Challenges and Rewards of a culturally-informed approach to mental health |Jessica Dere|TEDxUTSC [Video]. YouTube. https://www.youtube.com/watch?v=VrYmQDiunSc
Ask students to write their responses to the self-reflection questions on STUDENT HANDOUT 5 in their self-reflection journals.
Diverse Perceptions of Mental Health Challenges: Self-Reflection Journal
DIRECTIONS: After watching the video, Challenges and rewards of a culturally informed approach to mental health, answer the self-reflection questions below in your self-reflection journal.
Reflecting on cultural perspectives
- How do differences in cultural background and societal attitudes influence the perception of mental health challenges in diverse communities (consider stigmas and mental health)?
- How do differences in cultural background and societal attitudes influence access to health services and the willingness to seek help?
Reflect on a specific example from a particular group to illustrate your points.
Culturally safe and sensitive care
- What does it mean to take an approach of “informed curiosity” when providing culturally sensitive care?
- Why would this approach better promote cultural humility than an approach of being a knowledge expert?
Person-centred care
- How do the concepts of informed curiosity and culturally safe and sensitive care connect to the principle of providing person-centred care?
Personal and professional growth
Think about what your perceptions were toward mental health challenges before starting your program.
- How has your understanding of mental health in diverse groups changed since then?
- What experiences or knowledge have contributed to this change, and how do you think this will affect your approach to care?
3. Addressing Myths and Stigmas and Promoting Person-Centred Language
A. Anti-Stigma Videos
- As a homework activity, have students watch the video series on anti-stigma:
Provincial Health Services Authority. (2023). Anti-stigma [Video series]. YouTube. https://www.youtube.com/playlist?list=PLcE0nANeV5MrhI0CvgEQgWWmYE9F972GP
The series consists of six videos that will take about 35 minutes to view. - Alternatively, students could review other course information describing myths and stigma associated with dementia and mental health so they are prepared for the in-class discussion.
B. In-Class Discussion
- In class, discuss language and terms that contribute to myths and stigma.
C. Scenarios and Small Group Discussion
- Using the STUDENT HANDOUT 6 below, have students read the scenarios and work in partners or small groups and consider the following questions for each scenario:
- How do the language and actions presented in the scenario contribute to myths and stigma associated with dementia or mental health challenges?
- What do you think your immediate reaction to this situation would be?
- How could you use assertive communication to respond to the situation?
D. Whole Class Discussion
- After coming back together as a class, discuss possible responses to each situation, such as checking the behaviour immediately, paraphrasing back using person-centred language, gently explaining why the language is not appropriate, providing an alternative communication strategy.
STUDENT HANDOUT 6
Scenarios on Addressing Myths and Stigmas and Promoting Person-Centred Language
DIRECTIONS: Working in partners, read the scenarios and consider the following questions. Prepare to share your answers with the larger group:
- How do the language and actions presented in the scenario contribute to the myths and stigmas associated with dementia and/or mental health challenges?
- What do you think your immediate reaction to this situation would be?
- How could you use assertive communication to respond to the situation?
Scenario 1
You are an HCA working in an acute care setting. Mr. Namid, a 72-year-old man diagnosed with Alzheimer’s disease, has been admitted to the unit following a hip fracture. One of your colleagues has limited experience working with people who have dementia; you notice they tend to talk “over” Mr. Namid instead of including him in conversations. They also use terms such as “senile” and “demented” when referring to Mr. Namid.
Scenario 2
You are an HCA program graduate who has recently been hired at a complex care facility. When working with your new colleague, Alex, you notice that they refer to the number of “feeders” that they will be assisting during lunch.
Scenario 3
You are an HCA working in an assisted living home. You have been assigned to mentor Samir, who is an HCA student from a local college. One day while working with Samir, they refer to a client who is living with schizophrenia, as “the schizophrenic.”
Scenario 4
You are an HCA student working at your first clinical placement. One day, while working with a staff member named Mira, you refer to the client you are working with as a past “user.” Mira looks alarmed and rebukes you quite sharply for using this term.
4. Discussion on Abuse: Scenarios
- As a homework assignment, ask students to review the following pages on the B.C. Care Aide & Community Health Worker Registry (Registry) website:
- In class, review the information students reviewed on the Registry website.
- Ask students to visit the Reporting Alleged Abuse webpage and review the “Reportable Incidents” section, which includes definitions of abuse and neglect from the Community Care and Assisted Living Act.
- Using the STUDENT HANDOUT 7 below, have students work in partners or small groups to consider the following question for each scenario and response:
- Could this response be considered a reportable incident? By which definition?
- How do you think you would respond in this situation?
- What is an alternate response in this scenario?
- After coming back together as a class, discuss the alternate responses brought forward.
STUDENT HANDOUT 7
Discussion on Abuse: Scenarios
DIRECTIONS: Visit the B.C. Care Aide & Community Health Worker Reporting Alleged Abuse webpage. Review the “Reportable Incidents” section, which includes definitions of emotional abuse, financial abuse, neglect, physical abuse, and sexual abuse from the Community Care and Assisted Living Act Residential Care Regulation.
Working in pairs or small groups, read the scenarios and responses below. For each response, consider the following questions:
- Could this response be considered a reportable incident? By which definition?
- What do you think you would do if you observed this response?
- What is an alternate response to this scenario?
Be prepared to report back to the class.
Scenario 1
Mrs. Smith is a 92-year-old woman with dementia who is living in a complex care home. Today HCAs Jen and Mai are assigned to assist Mrs. Smith with morning care. When they enter her room, they observe that Mrs. Smith is still sleeping, and the room smells like she had a bowel movement. After greeting Mrs. Smith, Jen asks if she can turn on the light. Mrs. Smith declines, saying she wants to continue sleeping.
Responses:
- Wanting to ensure that Mrs. Smith gets cleaned up, Jen turns on the light and sets up her supplies. When Jen tries to engage Ms. Smith for morning care, she resists. Jen asks Mai to hold Mrs. Smith down while she provides care.
- Wanting to respect Mrs. Smith’s request, Mai suggests they move on to their next client. They return to Mrs. Smith three hours later, after they have assisted their remaining clients.
- Wanting to stay on track with client assignments, Jen sighs and responds, “Mrs. Smith, why are being so difficult? We have many other clients to help this morning. If you continue to hold things up, everyone will be annoyed with you.”
- Alternate response:
Scenario 2
Mr. Wong is an 83-year-old man who mobilizes by using a wheelchair and receives home support services. Today, Tim is the HCA assigned to assist Mr. Wong with his shower and make him lunch. This is the first time Tim has met Mr. Wong. When Tim arrives, Mr. Wong refuses to enter the bathroom with Tim and tells him that he will wait for his regular HCA to help him with his shower next week.
Responses:
- Wanting to put Mr. Wong at ease, Tim responds by saying that he is an experienced HCA, and everything will be fine. Tim wheels Mr. Wong to the bathroom and starts to unbutton his shirt. While Tim is doing so, Mr. Wong is crying and saying, “No, no, no!”
- Tim has a busy day and a lengthy commute to his next client. He agrees to Mr. Wong’s refusal, makes his lunch, and leaves for his next client.
- Knowing Mr. Wong has not had a bath since last week, Tim tells him that he is being difficult and does not smell very good. Tim tells Mr. Wong that if he does not cooperate, his family will not want to visit him.
- Alternate response:
Scenario 3
Mr. Singh is a home support client who has cognitive decline and requires support with his daily activities. Today, Carmen is the HCA assigned to help Mr. Singh with his bath. Today they finish ahead of schedule and Carmen has some extra time before her next client.
Responses:
- Carmen and Mr. Singh sit down for a visit. Carmen tells Mr. Singh her car is in the shop, and she is having to rely on ride-sharing services, which she cannot afford. Mr. Singh offers to pay for a ride-share service to get to her next client. This works so well that during the next visit, Mr. Singh signs Carmen up on his ride-share account.
- After Carmen has finished assisting Mr. Singh with his bath, he asks if Carmen will go to a nearby bank machine to take out some cash using his bank card. Carmen is short on cash and decides to take an extra $25.00 for her time.
- Mr. Singh asks if Carmen can go downstairs to find a photo album. While she is downstairs looking for the photo album, Carmen notices some earrings sitting on a dresser. She knows that Mr. Singh is rarely downstairs, and the family does not visit often. Mr. Singh has given her other gifts before. Carmen decides to take the earrings and does not tell Mr. Singh.
- Alternate response:
Scenario 4
Rohan is an HCA working his third night shift in a row. The unit is short-staffed, and Rohan is working alone for most of the night. Rohan is assigned to complete unit safety checks at 0100 and 0300 hours and to change the incontinence pads of four clients at 0530. Mrs. Taylor is having difficulty sleeping and keeps calling out for help. Rohan has several call bells to answer and feels tired and overwhelmed.
Responses:
- Rohan does not have time to keep responding to Mrs. Taylor. He tells her she is disturbing the other clients and closes her door.
- Rohan falls asleep at the nursing station and does not complete his 0300 safety check. He wakes up at 0400 and records that it was completed.
- Rohan only has time to change the pads for three of the four clients before the morning shift arrives. He was busy and it wasn’t his fault that the unit was short-staffed. He does not tell the morning shift that he ran out of time and did not assist the fourth client.
- Alternate response:
INSTRUCTOR DISCUSSION GUIDE 4
Discussions on Abuse: Scenarios
This learning activity is designed to help students critically evaluate HCA work scenarios, discuss whether the responses provided are reportable incidents related to abuse, and propose alternate strategies. It is an opportunity for students to review situations that HCAs may encounter in the workplace and emphasize the HCA’s role and responsibility for ensuring client safety.
- During this activity, students will discuss whether the responses provided for each scenario meet the following definitions of abuse as identified within the Community Care and Assisted Living Act Residential Care Regulation and posted to B.C. Care Aide & Community Health Worker Registry website.
- Emotional abuse: any act, or lack of action, which may diminish the sense of dignity of a person in care, perpetrated by a person not in care, such as verbal harassment, yelling or confinement
- Financial abuse: the misuse of the funds and assets of a person in care by a person not in care, or the obtaining of the property and funds of a person in care by a person not in care without the knowledge and full consent of the person in care or his or her parent or representative
- Neglect: the failure of a care provider to meet the needs of a person in care, including food, shelter, care, or supervision
- Physical abuse: any physical force that is excessive for, or is inappropriate to, a situation involving a person in care and perpetrated by a person in care
- Sexual abuse: any sexual behaviour directed towards a person in care and includes any sexual exploitation, whether consensual or not, by an employee of the licensee, or any other person in a position of trust, power or authority, and sexual activity between children or youths, but does not include consenting sexual behaviour between adult persons in care
- Students may have conflicting opinions on whether the responses fit these definitions. During their discussions, they may raise additional course concepts related to professional approaches to practice, including:
- DIPPS: Dignity, Independence, Individualized Care, Preferences, Privacy, Safety
- Ethical and legal parameters of the HCA role
- Employer policy (To support this activity, instructors are encouraged to source employer policies from their practice education partners that address related topics.)
- Students are invited to discuss how they would approach the situation and develop an alternative response to those provided. They will then discuss with the whole class and the instructor, who will be able to provide further insight regarding professional approaches to practice.
An example is provided below.
Example Responses to Scenario 2
Mr. Wong is an 83-year-old man who mobilizes by using a wheelchair and receives home support services. Today, Tim is the HCA assigned to assist Mr. Wong with his shower and make him lunch. This is the first time Tim has met Mr. Wong. When Tim arrives, Mr. Wong refuses to enter the bathroom with Tim and tells him that he will wait for his regular HCA to help him with his shower next week.
Responses:
A. Wanting to put Mr. Wong at ease, Tim responds by saying that he is an experienced HCA, and everything will be fine. Tim wheels Mr. Wong to the bathroom and starts to unbutton his shirt. While Tim is doing so, Mr. Wong is crying and saying, “No, no, no!”
For this response, students might discuss the following:
- Physical abuse, defined as “any physical force that is excessive for, or is inappropriate to, a situation involving a person in care and perpetrated by a person in care”
- Sexual abuse, defined as “any sexual behaviour directed towards a person in care and includes any sexual exploitation, whether consensual or not, by an employee of the licensee, or any other person in a position of trust, power or authority, and sexual activity between children or youths, but does not include consenting sexual behaviour between adult persons in care”
- Principles of DIPPS: Dignity, Independence, Privacy, and Preference
- Effective communication strategies
- Employer policies for reporting and recording
B. Tim has a busy day and a lengthy commute to his next client. He agrees to Mr. Wong’s refusal, makes his lunch, and leaves for his next client.
For this response, students might discuss neglect, defined as “the failure of a care provider to meet the needs of a person in care, including food, shelter, care, or supervision.
They may also discuss effective communication strategies, and employer policies for reporting and recording.”
C. Knowing Mr. Wong has not had a bath since last week, Tim tells him that he is being difficult and does not smell very good. Tim tells Mr. Wong that if he does not cooperate, his family will not want to visit him.
For this response, students might discuss emotional abuse, defined as “any act, or lack of action, which may diminish the sense of dignity of a person in care, perpetrated by a person not in care, such as verbal harassment, yelling or confinement.” Students may also discuss effective communication strategies, employer policies for bullying and harassment and employer policies for reporting and recording.
D. Alternate response:
Since this is the first time Mr. Wong and Tim have met, Mr. Wong might feel uncomfortable about having Tim assist him with his shower. Instead of starting with the bath, Tim could first make Mr. Wong some lunch and get to know him better. After lunch, Tim could ask Mr. Wong again if he could help him with his bath. Ultimately, if Mr. Wong refuses, Tim must respect Mr. Wong’s wishes and follow his employer’s policies on reporting and recording.
Suggested Course Assessments
The course learning outcomes may be assessed by the following tasks:
- One or more quizzes or exams that pertain to knowledge of common cognitive and/or mental health challenges, principles of crisis intervention, and elder abuse (Learning Outcomes 1, 2, 3, and 4).
- A written assignment that students will complete individually, based on interactions with a client with cognitive challenges (Learning Outcome 1). Refer to Responding to an Individual Experiencing Cognitive Challenged Assignment in Section 5: Sample Course Assessment Tools.
- Group presentation on supporting clients with dementia or a mental health disorder. Students can research and complete this project in small groups. They should put together a visual presentation (e.g., a poster, PowerPoint, or video) and a short written handout to give to the class. The focus should be on how to best communicate with and care for clients with dementia and/or mental health disorders. The online resources provided for this course will be particularly useful in preparing for this assignment (Learning Outcomes 1 and 2). Refer to Supporting Clients with Dementia or a Mental Health Disorder Group Presentation in Section 5: Sample Course Assessment Tools.
A variation of the assignment above could involve having the students focus on the physical, psychological, cognitive, and social changes that a person dealing with dementia or a mental health disorder might face. Each group should also identify community resources and be prepared to discuss the HCA role in supporting individuals and families (Learning Outcomes 1 and 2).
Resources for Cognitive and/or Mental Health Challenges
Online Resources
Alzheimer’s Association. (2021). Aggression and anger. https://www.alz.org/help-support/caregiving/stages-behaviors/agression-anger
Alzheimer’s Association. (2021). How the brain works: A tour of how the mind works. https://www.alz.org/alzheimers-dementia/what-is-alzheimers/brain_tour
Alzheimer’s Association. (2021). Inside the brain: A tour of how the mind works: Part 2-Alzheimer’s effect. https://www.alz.org/alzheimers-dementia/what-is-alzheimers/brain_tour_part_2
Alzheimer Society. (2019). Ambiguous loss and grief in dementia: A resource for individuals and families. https://alzheimer.ca/sites/default/files/documents/ambiguous-loss-and-grief_for-individuals-and-families.pdf
Alzheimer Society. (n.d.). Communicating with people living with dementia. https://alzheimer.ca/en/help-support/i-have-friend-or-family-member-who-lives-dementia/communicating-people-living-dementia
Alzheimer Society. (n.d.) Communication challenges and helpful strategies. https://alzheimer.ca/en/help-support/im-living-dementia/managing-changes-your-abilities/communication-challenges-helpful
Alzheimer Society. (2024). Dementia friendly communities Ontario. https://alzheimer.ca/on/en/take-action/become-dementia-friendly/dementia-friendly-communities-ontario
Alzheimer Society. (2017). Person-centred language guidelines. https://alzheimer.ca/sites/default/files/documents/Person-centred-language-guidelines_Alzheimer-Society.pdf
Alzheimer Society. (2017). Providing person-centred care. https://alzheimer.ca/en/help-support/im-healthcare-provider/providing-person-centred-care
Alzheimer Society. (n.d.). Restlessness or confusion, especially later in the day. https://alzheimer.ca/en/help-support/im-caring-person-living-dementia/understanding-symptoms/restlessness-or-confusion
Alzheimer Society. (2019). Supporting clients through ambiguous loss and grief. Strategies for healthcare providers. https://alzheimer.ca/sites/default/files/documents/Ambiguous%20Loss%20Health%20Provider%20En-20-FINAL-MD_1.pdf
Alzheimer Society. (2018). Understanding genetics and Alzheimer’s disease. https://alzheimer.ca/sites/default/files/documents/research_understanding-genetics-and-alzheimers-disease.pdf
Alzheimer Society British Columbia. https://alzheimer.ca/bc/en
Alzheimer Society British Columbia. (n.d.). Building a strong foundation for dementia care: health care provider education. https://alzheimer.ca/bc/sites/bc/files/documents/bsfdc-guidebook.pdf
Alzheimer Society Canada. https://alzheimer.ca/en
B.C. Mental Health and Substance Use Services. (2024). Trauma-informed practice. http://www.bcmhsus.ca/health-professionals/clinical-professional-resources/trauma-informed-practice
B.C. Ministry of Children and Family Development. (2017). Healing families, helping systems: Trauma-Informed practice guidelines for working with children, youth, and families. www2.gov.bc.ca/assets/gov/health/child-teen-mental-health/trauma-informed_practice_guide.pdf
B.C. Schizophrenia Society. https://www.bcss.org/
Blodget, T.J. (2023). Delirium prevention and management in hospitalized older adults. The Nurse Practitioner 48(5). 12–19. DOI:10.1097/01.NPR.0000000000000036
Canadian Alliance on Mental Illness and Mental Health. https://www.camimh.ca/
Canadian Association for Suicide Prevention. http://suicideprevention.ca/
Canadian Coalition for Senior’s Mental Health. https://ccsmh.ca/
Canadian Institute for Health Information. (n.d.). Dementia in Canada: Summary. https://www.cihi.ca/en/dementia-in-canada/dementia-in-canada-summary
Canadian Mental Health Association. http://www.cmha.ca/
Canadian Mental Health Association: Here to help. (2014). Learn about Alzheimer’s disease [Information sheet]. https://www.heretohelp.bc.ca/sites/default/files/alzheimers-disease.pdf
Canadian Mental Health Association. (2016). Myths about mental illness. http://www.cmha.ca/mental_health/myths-about-mental-illness/
Carreiro, D. (2013, October 15). Suicide rates climb among elderly in Canada. CBC News. https://www.cbc.ca/news/canada/manitoba/suicide-rates-climb-among-elderly-in-canada-1.2054402
Centre for Addiction and Mental Health. (2020). Trauma. https://www.camh.ca/en/health-info/mental-illness-and-addiction-index/trauma
Government of British Columbia. (2023, January 10). Protection from elder abuse and neglect. https://www2.gov.bc.ca/gov/content/family-social-supports/seniors/health-safety/protection-from-elder-abuse-and-neglect
Government of British Columbia, Ministry of Health. (2012, October 25). Best practice guideline for accommodating and managing behavioural and psychological symptoms of dementia in residential care. A person-centered interdisciplinary approach. https://www.health.gov.bc.ca/library/publications/year/2012/bpsd-guideline.pdf
HealthLinkBC. (2019). Dementia, British Columbia specific information. https://www.healthlinkbc.ca/health-topics/uf4984
HealthLinkBC. (2019). Dementia: Helping a person avoid confusion. http://www.healthlinkbc.ca/healthtopics/content.asp?hwid=hw135788
HealthLinkBC. (2018). Preventing abuse and neglect of older adults. https://www.healthlinkbc.ca/healthlinkbc-files/prevent-abuse-older-adults
Here to Help. (2019). Resource library. http://www.heretohelp.bc.ca/self-help-resources
Island Health. (2021). Mental health and substance use resources and education. https://www.islandhealth.ca/learn-about-health/mental-health/mental-health-substance-use-resources-education
MedicineNet. (2016). What are phobias? Agoraphobia, social anxiety disorder, other fears. https://www.medicinenet.com/phobias_picture_slideshow/article.htm
Mental Health Commission of Canada. (2020). Language matters. https://mentalhealthcommission.ca/resource/language-matters/
Mental Health Commission of Canada. (2023). Fact sheet: Common mental health myths and misconceptions. https://mentalhealthcommission.ca/resource/fact-sheet-common-mental-health-myths-and-misconceptions/
National Institute on Aging (NIH). (2023). Alzheimer’s disease genetics fact sheet. https://www.nia.nih.gov/health/genetics-and-family-history/alzheimers-disease-genetics-fact-sheet
Novilla-Surette, E.M.P., Shariff, S.Z., Le, B., Booth, R.G. (2022). Trends and factors associated with suicide deaths in older adults in Ontario, Canada. Canadian Geriatrics Journal, 25 (2). 134-161. doi: 10.5770/cgj.25.541 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9156420/
Office of the Seniors Advocate British Columbia. (2016, June). Resident to resident aggression in B.C. care homes. https://www.seniorsadvocatebc.ca/app/uploads/sites/4/2016/06/SA-ResidentToResidentAggressionReview-2016.pdf
PIECES. (n.d.). PIECES. Learning and development model. https://piecescanada.com/pages/learning-and-development
Programs for Elderly. (n.d.). Documentary library [Documentary films available as videos]. http://www.programsforelderly.com/index-documentaries-subpage.php
Schizophrenia Society of Canada. http://www.schizophrenia.ca
Seetharaman, K. & Chaudhury, H. (2020). Dementia-friendly care homes: Best practices in dementia care. https://bccare.ca/wp-content/uploads/2020/03/DFCH-Report_03_02web.pdf
Seniors First B.C. http://seniorsfirstbc.ca/
(Formerly the B.C. Centre for Elder Advocacy & Support)
Simon Fraser University, Centre for Applied Research in Mental Health and Addiction. http://www.sfu.ca/content/sfu/carmha.html
Smith, M. (2020). Caregiver stress and burnout. HelpGuide. https://www.helpguide.org/articles/stress/caregiver-stress-and-burnout.htm
UBC Student Health and Wellbeing Staff, Gillies, J., Johnston, B., Warwick, L., Devine, D., Guild, J., Hsu, A., Islam, H., Kaur, M., Mokhovikova, M., Nicholls, J. M., & Smith. C. (2021). The language of mental health. In Starting a conversation about mental health: Foundational training for students. BCcampus. https://opentextbc.ca/studentmentalhealth/chapter/the-language-of-mental-health/
University of Waterloo, Murray Alzheimer Research and Education Program. https://uwaterloo.ca/murray-alzheimer-research-and-education-program/
Validation Training Institute Inc. (n.d.). Getting started: Validation to suit your needs. https://vfvalidation.org/get-started/validation-to-suit-your-needs/#ui00c2e24|tab2
Wincer. P. (2020, November 26). What caring for my mum taught me about caring for my son. BBC News. https://www.bbc.com/news/stories-55057440
WorkSafeBC. (2010). Dementia: Understanding risks and preventing violence. https://www.worksafebc.com/en/resources/health-safety/books-guides/dementia-understanding-risks-and-preventing-violence?lang=en
WorkSafeBC. (n.d.) Working with people with dementia. https://www.worksafebc.com/en/health-safety/industries/health-care-social-services/topics/working-with-people-with-dementia
Zhou, Z. (2023). Canada’s first publicly funded “dementia village” is set to open next year. So, what is it?” https://healthydebate.ca/2023/06/topic/publicly-funded-dementia-village/
Online Videos
AJ+. (2015). If you’re not white it’s harder to get mental health care [Video]. YouTube. https://www.youtube.com/watch?v=FgNaqfGTysU
Alzheimer’s Research Association. (2020, November 19). Former ballerina with Alzheimer’s performs ‘Swan Lake’ dance: super emotional [Video]. YouTube. https://www.youtube.com/watch?v=IT_tW3EVDK8
Alzheimer’s WA. (2019, August 15). Person-centered care in dementia [Video]. YouTube. https://youtu.be/o0jpWKjYwHg?si=Ycxilmbn1qxpcbzc
Alzheimer’s Society. (2020, September 17). Understanding dementia: progression and symptoms [Video]. YouTube. https://youtu.be/cT-xTqE5ZFE?si=aFCV_xmIyCuWdkX
Alzheimer’s Society of BC. (2020, Sept 2017). Understanding dementia: The brain and dementia [Video]. YouTube. https://youtu.be/XLBERzsWwGo?si=uzM_6KE9BvFCSmAo
Alzheimer’s Society of Canada. (2022, March 21). What is a dementia-friendly community? [Video]. YouTube. https://www.youtube.com/watch?v=rTM4RCmUgK4
Alzheimer’s Society. (2017, January 26). What is Alzheimer’s disease? [Video]. YouTube. https://youtu.be/wfLP8fFrOp0?si=L5w2JqQ2rRB_7HSA
Animated Alzheimer’s Patient. (2021, January 27). Understanding Alzheimer’s disease [Video]. YouTube. https://www.youtube.com/watch?v=lFBTlHfV8Iw
Applewhite, A. (2017, April). Let’s end ageism [Video]. TED2017. https://www.ted.com/talks/ashton_applewhite_let_s_end_ageism
BC Schizophrenia Society. (2022, April 5). Symptoms of schizophrenia (Overview) [Video]. YouTube. https://youtu.be/9DHKoBUZtq0?si=cymZ0WjLrNz2bNZB
Being Patient Alzheimer’s. (2019, April 19) Robotic pets to the rescue? Dementia care gets innovative / being patient [Video]. YouTube. https://youtu.be/F_WBTLWUIfM?si=1aDTEu2PZS7SBpNO
Big Think. (2022, July 8). 5 ways to build an Alzheimer’s resistant brain. Lisa Genova [Video]. YouTube. https://youtu.be/xBDGgovA1LI?si=AIXSxob9c-5GuTpp
Brenda Curtwright and Associates. (2022, May 14). Reminiscence therapy. Engaging long-term memories for people with dementia [Video]. YouTube. https://www.youtube.com/watch?v=Wh5esQHFNAs
CBC News: The National. (2015, October 11). Home recreates past for dementia patients [Video]. YouTube. https://www.youtube.com/watch?v=9rOYmxIWzJI
CBC News: The National. (2015, August 4). Seniors home brings young and old together [Video]. YouTube. https://www.youtube.com/watch?v=3LGSfgOi9UU
CNN. (2014, June 9). Anderson Cooper tries a schizophrenic simulator [Video]. YouTube. https://www.youtube.com/watch?v=yL9UJVtgPZY
Covenant Health Canada. (2019, May 31). Busy blankets calm residents with dementia [Video]. YouTube. https://www.youtube.com/watch?v=gcWsTsYC5s0
Creative Connections. (2016, May 17). Delirium awareness video [Video]. YouTube. https://www.youtube.com/watch?v=BPfZgBmcQB8
Dementia Care Hub. (2023, January 26). Sensory activities for dementia: Simple activities with big benefits [Video]. YouTube. https://www.youtube.com/watch?v=lTGd0tenwzY
Dementia Spring. (2019, June 13). Do people die of dementia? Dr.Marc [Video]. YouTube. https://www.youtube.com/watch?v=gEF7TolL9IQ
Demystifying Medicine McMaster. (2018, November 11). Art therapy. A potential treatment for dementia [Video]. YouTube.https://www.youtube.com/watch?v=Ro_xTd-Ugzw
Durham University. (2021, October 18). Infrared light therapy might aid people with dementia [Video]. YouTube. https://www.youtube.com/watch?v=J6JsE-VabPA
Education for Rural and Underserved Communities. (2016, April 8). Persons with dementia: Skills for addressing challenging behaviors [Video]. YouTube. https://www.youtube.com/watch?v=hgVMKEnkvHo
French Connection Films. (2009, November 4). I remember better when I paint [Video]. YouTube. https://www.youtube.com/watch?v=54AtoQVGfwU
Global News. (2023, May 6) Inside Canada’s first dementia village [Video]. YouTube. https://youtu.be/7A39UmdGmLQ?si=-rXo_ZESViNPz7eM
Havethattalk. (2019, Mar 18). Mental health = health (for diverse communities) [Video]. YouTube. https://www.youtube.com/watch?v=Izp4lZcJoSQ
Havethattalk. (2017, May 3). Reducing stigma [Video]. YouTube. https://www.youtube.com/watch?v=eio-I8PbdDk
Healthy Canadians. (2023, Feb 23). Dementia risk reduction – Physical inactivity [Video]. https://www.canada.ca/en/public-health/services/video/dementia-risk-reduction-physical-inactivity.html
Healthy Canadians. (2023, Feb 23). Dementia risk reduction – High blood pressure. [Video]. YouTube. https://youtu.be/KvrMWqFICoE?si=iSGZGtTAOqkE8ZMY
Healthy Canadians. (2024, January 29). Supports for dealing with mental health challenges [Video]. YouTube. https://youtu.be/IR1nISWZ7o8?si=xIoS-HObZ2BMOWWA
Island Health. (Jan 8, 2019). Dementia caregiving environmental adaptations. [Video]. https://www.youtube.com/watch?v=6Xb-Nlou_Co
Kujath, J. (2017, November 16). Understanding cycles of abuse [Video]. YouTube. https://youtu.be/0Q0-Eps1ThE
Martin, G. (2015, June 22). How to approach residents with behaviors [Video]. YouTube. https://www.youtube.com/watch?v=xylQt7TxDwo
Memorybridge. (2009, May 26). Gladys Wilson and Naomi Feil [Video]. YouTube. https://www.youtube.com/watch?v=CrZXz10FcVM
Mental Health at Work. (2016, July 1). What is mental health? [Video]. YouTube. https://www.youtube.com/watch?v=G0zJGDokyWQ4
Miller, B. (2015, March). What really matters at the end of life [Video]. TED2015. https://www.ted.com/talks/bj_miller_what_really_matters_at_the_end_of_life
Mmlearn. (2018, September 28). How to talk to someone with dementia: Diane Waugh [Video]. YouTube. https://www.youtube.com/watch?v=ilickabmjww
Music and Memory. (2011, November 18). Man in nursing home reacts to music from his era [Video]. YouTube. https://youtu.be/fyZQf0p73QM
SafeCare B.C. (2019, February 5). Dementia care teams: Families and continuing care providers working together [Video]. YouTube. https://www.youtube.com/watch?app=desktop&v=VxDopCVswmg
Saks, E. (2012, June). A tale of mental illness from the inside [Video]. TEDGlobal2012. https://www.ted.com/talks/elyn_saks_seeing_mental_illness
StoryHive. (2015, April 17). Journey through Alzheimer’s: Late stages. [Video]. YouTube. https://www.youtube.com/watch?v=lBNRhHDSUXY0
TED. (2017, May 19). What can you do to prevent Alzheimer’s disease: Lisa Genova [Video]. YouTube. https://www.youtube.com/watch?v=twG4mr6Jov0
TEDx Talks. (2012, October 9). The power of addiction and the addiction of power: Gabor Maté at TED [Video]. YouTube. https://www.youtube.com/watch?v=66cYcSak6nE
TEDx Talks. (2017, March 27). I am not a monster: Schizophrenia – Cecilia McGough. TEDxPSU [Video]. YouTube. https://www.youtube.com/watch?v=xbagFzcyNiM
Validation Theory Institute. (2017, March 13). What is validation – Interview by Naomi Feil [Video]. YouTube. https://www.youtube.com/watch?v=ejVqVKWnDOE
Online Learning Tools
The following materials are ready for use in the classroom or online. A brief description and estimated time to complete each activity is included for each.
Island Health. (n.d.). Dementia video series: Practical advice from caregivers, for caregivers.
- A variety of videos and resources about dementia and caregiving (approximately 10 minutes per video).
LearningHub, Provincial Health Services Authority
LearningHub is a secure, province-wide course registry and learning management system hosted by the Provincial Health Services Authority. LearningHub provides a wide range of online and in-class courses on various topics. These e-learning courses can be used as activities or assessments for the HCA program courses. Students can access the LearningHub using their post-secondary email account. After completing all mandatory learning activities for a course, students can obtain a course completion certificate to show that they fulfilled all the course requirements. Instructions for registering and completing courses are available on the LearningHub site.
The following courses are examples of courses related to dementia, mental health, and person-centred care. All courses are accessible to HCA students.
- Dementia Care: Fundamental Knowledge, Skills and Competencies for Providing Person-Centered Care. (3 hours)
- Mental Health Act – Island Health (1 hour)
- Patient-Centred Approach to Dementia Care: Dementia Care Gamification eLearning
- Resisting Stigma on Substance Use (40 minutes)
- Supporting Sexual Health & Intimacy in LTC, Assisted Living, Group Homes and Supported Housing (45 minutes)
Note: The above module is recommended in conjunction with the debate question on supporting clients with dementia in romantic or sexual relationships. Students could be asked to participate in a debate or research to support their assigned perspectives. After the debate, all students could be assigned to complete this module.
Maté, Gabor. (2024). Trauma.
- This website offers several sections on mental health including trauma, addiction, and the mind/body connection. The site includes many articles, interviews, audio recordings and videos on trauma. Most of the content is available for free, although some require subscriptions. Students could be asked to review one of the resources and then provide a summary of it during a small group discussion.
Province of British Columbia. (2015). Elder abuse reduction curricular resource. BCcampus.
- An instructor’s guide and a presentation for teaching core competencies in elder abuse prevention, detection, and response in B.C. Within the guide, there are activities, assignments, online video links, readings and evaluation questions, as well as references to additional resources for some topic areas.
Provincial Health Services Authority. (2023). Anti-stigma [Video series].
- This animated video series includes two three-part video series: Stories of Experience and Stories of Family Experience. The videos include personal stories of individuals’ experiences with mental health and how stigma within the health care system has influenced their lives. The series was a partnership between BC Mental Health and Substance Use Services and Emily Carr University to give individuals the opportunity to share their experiences through storytelling.
- There are six videos, and each video is around 5–6 minutes in length with a total length of around 35 minutes.
- This video series is recommended for the activity Addressing Myths and Stigmas.
OC87 Recovery Diaries. (2020). Writers talk mental health [Videos].
- This video series includes personal stories of struggles with mental health challenges, empowerment, and change. The videos present a range of experiences, including the connection between writing and mental health recovery, trauma and stigma. Each story is told by an individual from a different country, thus also bringing into consideration the presence of mental health challenges across diverse groups. The mental health challenges included in the series are anxiety, depression, bipolar disorder and obsessive-compulsive disorder.
- Each video is around 3 to4 minutes in length with a total length of around 15–20 minutes.
- This video series could be embedded into the lecture content when presenting on the curriculum topic of “common mental health disorders” and/or paired with discussion questions or a self-reflection journal question.
Ontario CLRI. (2018). Dementia simulation toolkit.
- The Ontario Centres for Learning, Research and Innovation in Long-Term Care website provides a simulation toolkit designed to enhance knowledge, value and attitudes regarding dementia in students. The scripts and resources provided are designed to build student awareness and insight into the lives of persons living with dementia and frailty.
Registered Nurses ‘Association of Ontario. (2017). RNAO Nurse Educator: Mental Health and Additional Resource.
- This website includes nine sections providing information, resources, case studies, journaling topics and discussion questions to help support the teaching of mental health, mental health care in nursing, and trauma-informed care. Three subsections are highlighted below.
- 5.3 Trauma-Informed Care Teaching Activities and Resources.
- 9.3 Case Studies (includes questions for discussion or written reflection)
- 2.3 Tool #2: Educator Self-Assessment
Rossato-Bennett, M., McDougald, A., Scully, R. K., Cohen, D., Sacks, O., McFerrin, B., Shur, I. (2014). Alive inside: A story of music and memory. MVD Visual (Film).
- This film can be used as part of a larger discussion on the importance of person-centred care, dementia, and music (77 minutes).
TEDEd. (2017). TED-Ed Lessons about mental health.
- A series of eight videos about symptoms and treatments for eight mental health challenges, including depression, bipolar disorder, and schizophrenia. The series also includes a video on stress and mental health and a video on the use of electroconvulsive therapy in mental health.
Teepa Snow’s Positive Approach to Care. [YouTube Channel]
- This YouTube site provides over 900 videos regarding dementia and care strategies for persons with dementia. Six videos from this channel have been highlighted below.
- Teepa Snow. (2023, May 18). Dementia care tips for hygiene, bathing support, and validation.
- Teepa Snow. (2017, April 29). Challenging behaviors and dementia.
- Teepa Snow. (2017, De 21). Dementia 101.
- Teepa Snow. (2017, Dec 21). Connecting through music in dementia care.
- Teepa Snow. (2023, July 27). How can we de-escalate someone that is agitated?.
- Teepa Snow. (2017, Dec 21). Meaningful activities and dementia.
WorkSafeBC. (2013). Two-person care needs a planned approach [Video].
- A video and discussion guide about how planning two-person care can reduce risk (10–15 minutes).
WorkSafeBC. (2009). Working with dementia: Safe work practices for caregivers [Videos].
- A series of six videos and a discussion guide describing how to care for people with dementia (each video is 10–15 minutes).

