Chapter 13. Defining Psychological Disorders
13.3 Mood Disorders: Emotions as Illness
Learning Objectives
- Summarize and differentiate the various forms of mood disorders, in particular dysthymia, major depressive disorder, and bipolar disorder.
- Explain the genetic and environmental factors that increase the likelihood that a person will develop a mood disorder.
The everyday variations in our feelings of happiness and sadness reflect our mood, which can be defined as the positive or negative feelings that are in the background of our everyday experiences. In most cases we are in a relatively good mood, and this positive mood has some positive consequences — it encourages us to do what needs to be done and to make the most of the situations we are in (Isen, 2003). When we are in a good mood our thought processes open up, and we are more likely to approach others. We are more friendly and helpful to others when we are in a good mood than we are when we are in a bad mood, and we may think more creatively (De Dreu, Baas, & Nijstad, 2008). On the other hand, when we are in a bad mood we are more likely to prefer to be alone rather than interact with others, we focus on the negative things around us, and our creativity suffers.
It is not unusual to feel down or low at times, particularly after a painful event such as the death of someone close to us, a disappointment at work, or an argument with a partner. We often get depressed when we are tired, and many people report being particularly sad during the winter when the days are shorter. Mood (or affective) disorders are psychological disorders in which the person’s mood negatively influences his or her physical, perceptual, social, and cognitive processes. People who suffer from mood disorders tend to experience more intense — and particularly more intense negative — moods. About 5% of the Canadian population suffers from a mood disorder in a given year (Health Canada, 2002).
The most common symptom of mood disorders is negative mood, also known as sadness or depression (Figure 13.9, “Depression”). Consider the feelings of this person, who was struggling with depression and was diagnosed with major depressive disorder:
I didn’t want to face anyone; I didn’t want to talk to anyone. I didn’t really want to do anything for myself…I couldn’t sit down for a minute really to do anything that took deep concentration…It was like I had big huge weights on my legs and I was trying to swim and just kept sinking. And I’d get a little bit of air, just enough to survive and then I’d go back down again. It was just constantly, constantly just fighting, fighting, fighting, fighting, fighting. (National Institute of Mental Health, 2010)

Mood disorders can occur at any age, and the median age of onset is 32 years (Kessler, Berglund, Demler, Jin, & Walters, 2005). Recurrence of depressive episodes is fairly common and is greatest for those who first experience depression before the age of 15 years. About twice as many women as men suffer from depression (Culbertson, 1997). This gender difference is consistent across many countries and cannot be explained entirely by the fact that women are more likely to seek treatment for their depression. Rates of depression have been increasing, although the reasons for this increase are not known (Kessler et al., 2003).
As you can see in the list below, the experience of depression has a variety of negative effects on our behaviours. In addition to the loss of interest, productivity, and social contact that accompanies depression, the person’s sense of hopelessness and sadness may become so severe that he or she considers or even succeeds in committing suicide. In 2009 there were 3,890 suicides in Canada, a rate of 11.5 per 100,000 (Navaneelan, 2012). Almost all the people who commit suicide have a diagnosable psychiatric disorder at the time of their death (Statistics Canada, 2012; Sudak, 2005).
Behaviours Associated with Depression
- Changes in appetite; weight loss or gain
- Difficulty concentrating, remembering details, and making decisions
- Fatigue and decreased energy
- Feelings of hopelessness, helplessness, and pessimism
- Increased use of alcohol or drugs
- Irritability, restlessness
- Loss of interest in activities or hobbies once pleasurable, including sex
- Loss of interest in personal appearance
- Persistent aches or pains, headaches, cramps, or digestive problems that do not improve with treatment
- Sleep disorders, either trouble sleeping or excessive sleeping
- Thoughts of suicide or attempts at suicide
Dysthymia and Major Depressive Disorder
The level of depression observed in people with mood disorders varies widely. People who experience depression for many years, to the point that it becomes to seem normal and part of their everyday life, and who feel that they are rarely or never happy, will likely be diagnosed with a mood disorder. If the depression is mild but long-lasting, they will be diagnosed with dysthymia, a condition characterized by mild, but chronic, depressive symptoms that last for at least two years.
If the depression continues and becomes even more severe, the diagnosis may become that of major depressive disorder. Major depressive disorder (clinical depression) is a mental disorder characterized by an all-encompassing low mood accompanied by low self-esteem and loss of interest or pleasure in normally enjoyable activities. Those who suffer from major depressive disorder feel an intense sadness, despair, and loss of interest in pursuits that once gave them pleasure. These negative feelings profoundly limit the individual’s day-to-day functioning and ability to maintain and develop interests in life (Fairchild & Scogin, 2008).
About 4.8% of Canadian adults suffer from a major depressive disorder in any given year. Major depressive disorder occurs about twice as often in women as it does in men (Kessler, Chiu, Demler, & Walters, 2005; Kessler et al., 2003). In some cases clinically depressed people lose contact with reality and may receive a diagnosis of major depressive episode with psychotic features. In these cases the depression includes delusions and hallucinations.
Bipolar Disorder
Juliana is a 21-year-old single woman. Over the past several years she had been treated by a psychologist for depression, but for the past few months she had been feeling a lot better. Juliana had landed a good job in a law office and found a steady boyfriend. She told her friends and parents that she had been feeling particularly good — her energy level was high and she was confident in herself and her life.
One day Juliana was feeling so good that she impulsively quit her new job and left town with her boyfriend on a road trip. But the trip didn’t turn out well because Juliana became impulsive, impatient, and easily angered. Her euphoria continued, and in one of the towns that they visited she left her boyfriend and went to a party with some strangers that she had met. She danced into the early morning and ended up having sex with several of the men.
Eventually Juliana returned home to ask for money, but when her parents found out about her recent behaviour and confronted her, she acted aggressively and abusively to them, so they referred her to a social worker. Juliana was hospitalized, where she was diagnosed with bipolar disorder.
While dysthymia and major depressive disorder are characterized by overwhelming negative moods, bipolar disorder is a psychological disorder characterized by swings in mood from overly “high” to sad and hopeless, and back again, with periods of near-normal mood in between. Bipolar disorder is diagnosed in cases such as Juliana’s, where experiences with depression are followed by a more normal period and then a period of mania or euphoria in which the person feels particularly awake, alive, excited, and involved in everyday activities but is also impulsive, agitated, and distracted. Without treatment, it is likely that Juliana would cycle back into depression and then eventually into mania again, with the likelihood that she would harm herself or others in the process.
Based on his intense bursts of artistic productivity (in one two-month period in 1889 he produced 60 paintings), personal writings, and behaviour (including cutting off his own ear), it is commonly thought that Vincent van Gogh suffered from bipolar disorder. He committed suicide at age 37 (Thomas & Bracken, 2001). His painting, Starry Night, is shown in Figure 13.10.
Bipolar disorder is an often chronic and lifelong condition that may begin in childhood. Although the normal pattern involves swings from high to low, in some cases the person may experience both highs and lows at the same time. Determining whether a person has bipolar disorder is difficult due to the frequent presence of comorbidity with both depression and anxiety disorders. Bipolar disorder is more likely to be diagnosed when it is initially observed at an early age, when the frequency of depressive episodes is high, and when there is a sudden onset of the symptoms (Bowden, 2001).
Explaining Mood Disorders
Mood disorders are known to be at least in part genetic, because they are heritable (Berrettini, 2006; Merikangas et al., 2002). Neurotransmitters also play an important role in mood disorders. Serotonin, dopamine, and norepinephrine are all known to influence mood (Sher & Mann, 2003), and drugs that influence the actions of these chemicals are often used to treat mood disorders.
The brains of those with mood disorders may in some cases show structural differences from those without them. Videbech and Ravnkilde (2004) found that the hippocampus was smaller in depressed subjects than in normal subjects, and this may be the result of reduced neurogenesis (the process of generating new neurons) in depressed people (Warner-Schmidt & Duman, 2006). Antidepressant drugs may alleviate depression in part by increasing neurogenesis (Duman & Monteggia, 2006).
Research Focus: Using Molecular Genetics to Unravel the Causes of Depression
Avshalom Caspi and his colleagues (Caspi et al., 2003) used a longitudinal study to test whether genetic predispositions might lead some people, but not others, to suffer from depression as a result of environmental stress. Their research focused on a particular gene, the 5-HTT gene, which is known to be important in the production and use of the neurotransmitter serotonin. The researchers focused on this gene because serotonin is known to be important in depression, and because selective serotonin reuptake inhibitors (SSRIs) have been shown to be effective in treating depression.
People who experience stressful life events, for instance involving threat, loss, humiliation, or defeat, are likely to experience depression. But biological-situational models suggest that a person’s sensitivity to stressful events depends on his or her genetic makeup. The researchers therefore expected that people with one type of genetic pattern would show depression following stress to a greater extent than people with a different type of genetic pattern.
The research included a sample of 1,037 adults from Dunedin, New Zealand. Genetic analysis on the basis of DNA samples allowed the researchers to divide the sample into two groups on the basis of the characteristics of their 5-HTT gene. One group had a short version (or allele) of the gene, whereas the other group did not have the short allele of the gene.
The participants also completed a measure where they indicated the number and severity of stressful life events that they had experienced over the past five years. The events included employment, financial, housing, health, and relationship stressors. The dependent measure in the study was the level of depression reported by the participant, as assessed using a structured interview test (Robins, Cottler, Bucholtz, & Compton, 1995).
As you can see in Figure 13.11 as the number of stressful experiences the participants reported increased from 0 to 4, depression also significantly increased for the participants with the short version of the gene (top panel). But for the participants who did not have a short allele, increasing stress did not increase depression (bottom panel). Furthermore, for the participants who experienced four stressors over the past five years, 33% of the participants who carried the short version of the gene became depressed, whereas only 17% of participants who did not have the short version did.
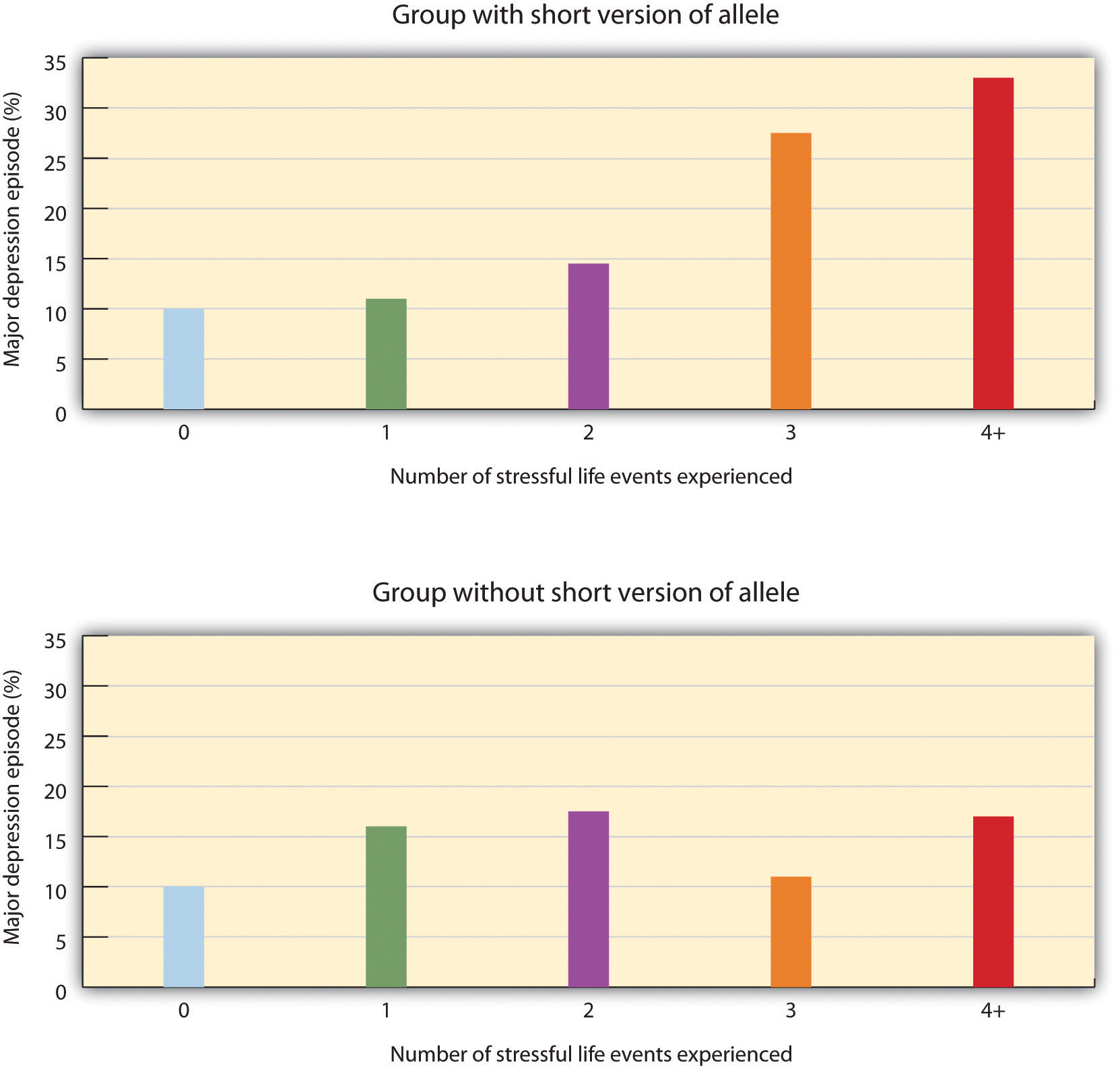
This important study provides an excellent example of how genes and environment work together: an individual’s response to environmental stress was influenced by his or her genetic makeup.
But psychological and social determinants are also important in creating mood disorders and depression. In terms of psychological characteristics, mood states are influenced in large part by our cognitions. Negative thoughts about ourselves and our relationships to others create negative moods, and a goal of cognitive therapy for mood disorders is to attempt to change people’s cognitions to be more positive. Negative moods also create negative behaviours toward others, such as acting sad, slouching, and avoiding others, which may lead those others to respond negatively to the person, for instance by isolating that person, which then creates even more depression (Figure 13.12, “Cycle of Depression”). You can see how it might become difficult for people to break out of this “cycle of depression.”

Weissman et al. (1996) found that rates of depression varied greatly among countries, with the highest rates in European and North American countries and the lowest rates in Asian countries. These differences seem to be due to discrepancies between individual feelings and cultural expectations about what one should feel. People from European and North American cultures report that it is important to experience emotions such as happiness and excitement, whereas the Chinese report that it is more important to be stable and calm. Because North Americans may feel that they are not happy or excited but that they are supposed to be, this may increase their depression (Tsai, Knutson, & Fung, 2006).
Key Takeaways
- Mood is the positive or negative feelings that are in the background of our everyday experiences.
- We all may get depressed in our daily lives, but people who suffer from mood disorders tend to experience more intense — and particularly more intense negative — moods.
- The most common symptom of mood disorders is negative mood.
- If a person experiences mild but long-lasting depression, he or she will be diagnosed with dysthymia. If the depression continues and becomes even more severe, the diagnosis may become that of major depressive disorder.
- Bipolar disorder is characterized by swings in mood from overly “high” to sad and hopeless, and back again, with periods of near-normal mood in between.
- Mood disorders are caused by the interplay among biological, psychological, and social variables.
Exercises and Critical Thinking
- Give a specific example of the negative cognitions, behaviours, and responses of others that might contribute to a cycle of depression like that shown in Figure 13.12, “Cycle of Depression.”
- Given the discussion about the causes of negative moods and depression, what might people do to try to feel better on days that they are experiencing negative moods?
References
Berrettini, W. (2006). Genetics of bipolar and unipolar disorders. In D. J. Stein, D. J. Kupfer, & A. F. Schatzberg (Eds.), Textbook of mood disorders. Washington, DC: American Psychiatric Publishing.
Bowden, C. L. (2001). Strategies to reduce misdiagnosis of bipolar depression. Psychiatric Services, 52(1), 51–55.
Caspi, A., Sugden, K., Moffitt, T. E., Taylor, A., Craig, I. W., Harrington, H.,…Poulton, R. (2003). Influence of life stress on depression: Moderation by a polymorphism in the 5-HTT gene. Science, 301(5631), 386–389.
Culbertson, F. M. (1997). Depression and gender: An international review. American Psychologist, 52, 25–31.
De Dreu, C. K. W., Baas, M., & Nijstad, B. A. (2008). Hedonic tone and activation level in the mood-creativity link: Toward a dual pathway to creativity model. Journal of Personality and Social Psychology, 94(5), 739–756.
Duman, R. S., & Monteggia, L. M. (2006). A neurotrophic model for stress-related mood disorders. Biological Psychiatry, 59, 1116–1127.
Fairchild, K., & Scogin, F. (2008). Assessment and treatment of depression. In K. Laidlow & B. Knight (Eds.), Handbook of emotional disorders in later life: Assessment and treatment. New York, NY: Oxford University Press.
Health Canada. (2002). A Report on Mental Illnesses in Canada. Ottawa, Canada. Retrieved July 2014 from http://www.phac-aspc.gc.ca/publicat/miic-mmac/chap_2-eng.php
Isen, A. M. (2003). Positive affect as a source of human strength. In J. Aspinall, A psychology of human strengths: Fundamental questions and future directions for a positive psychology (pp. 179–195). Washington, DC: American Psychological Association.
Kessler, R. C., Berglund, P. A., Demler, O., Jin, R., & Walters, E. E. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R). Archives of General Psychiatry, 62(6), 593–602.
Kessler, R. C., Berglund, P., Demler, O, Jin, R., Koretz, D., Merikangas, K. R.,…Wang, P. S. (2003). The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS-R). Journal of the American Medical Association, 289(23), 3095–3105.
Kessler, R. C., Chiu, W. T., Demler, O., & Walters, E. E. (2005). Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 617–27.
Merikangas, K., Chakravarti, A., Moldin, S., Araj, H., Blangero, J., Burmeister, M,…Takahashi, A. S. (2002). Future of genetics of mood disorders research. Biological Psychiatry, 52(6), 457–477.
National Institute of Mental Health. (2010, April 8). People with depression discuss their illness. Retrieved from http://www.nimh.nih.gov/media/video/health/depression.shtml
Navaneelan, T. (2012). Health at a Glance: Suicide rates: an overview. Statistics Canada. Retrieved 2014 from http://www.statcan.gc.ca/pub/82-624-x/2012001/article/11696-eng.htm
Robins, L. N., Cottler, L., Bucholtz, K., & Compton, W. (1995). Diagnostic interview schedule for DSM-1V. St. Louis, MO: Washington University.
Sher, L., & Mann, J. J. (2003). Psychiatric pathophysiology: Mood disorders. In A. Tasman, J. Kay, & J. A. Lieberman (Eds.), Psychiatry. New York, NY: John Wiley & Sons.
Statistics Canada. (2012). Suicides and suicide rate by sex and age group. Retrieved July 2014 from http://www.statcan.gc.ca/tables-tableaux/sum-som/l01/cst01/hlth66a-eng.htm
Sudak, H. S. (2005). Suicide. In B. J. Sadock & V. A. Sadock (Eds.), Kaplan & Sadock’s comprehensive textbook of psychiatry. Philadelphia, PA: Lippincott Williams & Wilkins.
Thomas, P., & Bracken, P. (2001). Vincent’s bandage: The art of selling a drug for bipolar disorder. British Medical Journal, 323, 1434.
Tsai, J. L., Knutson, B., & Fung, H. H. (2006). Cultural variation in affect valuation. Journal of Personality and Social Psychology, 90, 288–307.
Videbech, P., & Ravnkilde, B. (2004). Hippocampal volume and depression: A meta-analysis of MRI studies. American Journal of Psychiatry, 161, 1957–1966.
Warner-Schmidt, J. L., & Duman, R. S. (2006). Hippocampal neurogenesis: Opposing effects of stress and antidepressant treatment. Hippocampus, 16, 239–249.
Weissman, M. M., Bland, R. C., Canino, G. J., Greenwald, S., Hwu, H-G., Joyce, P. R., Yeh, E-K. (1996). Cross-national epidemiology of major depression and bipolar disorder. Journal of the American Medical Association, 276, 293–299.
Image Attributions
Figure 13.9: “sad looking woman” by Bradley Gordon is licensed under CC BY 2.0 license (http://creativecommons.org/licenses/by/2.0/deed.en_CA)
Figure 13.11: Adapted from Caspi, A., et al., 2003.
Long Description
| Number of stressful life events experienced | Major Depression Episode (%) | |
|---|---|---|
| Group with short version of allele | Group without short version of allele | |
| 0 | 10% | 10% |
| 1 | 11% | 16% |
| 2 | 14% | 18% |
| 3 | 28% | 11% |
| 4 or more | 33% | 18% |