Chapter 11: Introduction to the Body’s Systems
11.5 Musculoskeletal System
Learning Objectives
By the end of this section, you will be able to:
- Discuss the axial and appendicular parts of the skeletal system
- Explain the role of joints in skeletal movement
- Explain the role of muscles in locomotion=
The muscular and skeletal systems provide support to the body and allow for movement. The bones of the skeleton protect the body’s internal organs and support the weight of the body. The muscles of the muscular system contract and pull on the bones, allowing for movements as diverse as standing, walking, running, and grasping items.
Injury or disease affecting the musculoskeletal system can be very debilitating. The most common musculoskeletal diseases worldwide are caused by malnutrition, which can negatively affect development and maintenance of bones and muscles. Other diseases affect the joints, such as arthritis, which can make movement difficult and, in advanced cases, completely impair mobility.
Progress in the science of prosthesis design has resulted in the development of artificial joints, with joint replacement surgery in the hips and knees being the most common. Replacement joints for shoulders, elbows, and fingers are also available.
Skeletal System
The human skeleton is an endoskeleton that consists of 206 bones in the adult. An endoskeleton develops within the body rather than outside like the exoskeleton of insects. The skeleton has five main functions: providing support to the body, storing minerals and lipids, producing blood cells, protecting internal organs, and allowing for movement. The skeletal system in vertebrates is divided into the axial skeleton (which consists of the skull, vertebral column, and rib cage), and the appendicular skeleton (which consists of limb bones, the pectoral or shoulder girdle, and the pelvic girdle).
Concept in Action

Explore the human skeleton by viewing the following video with digital 3D sculpturing.
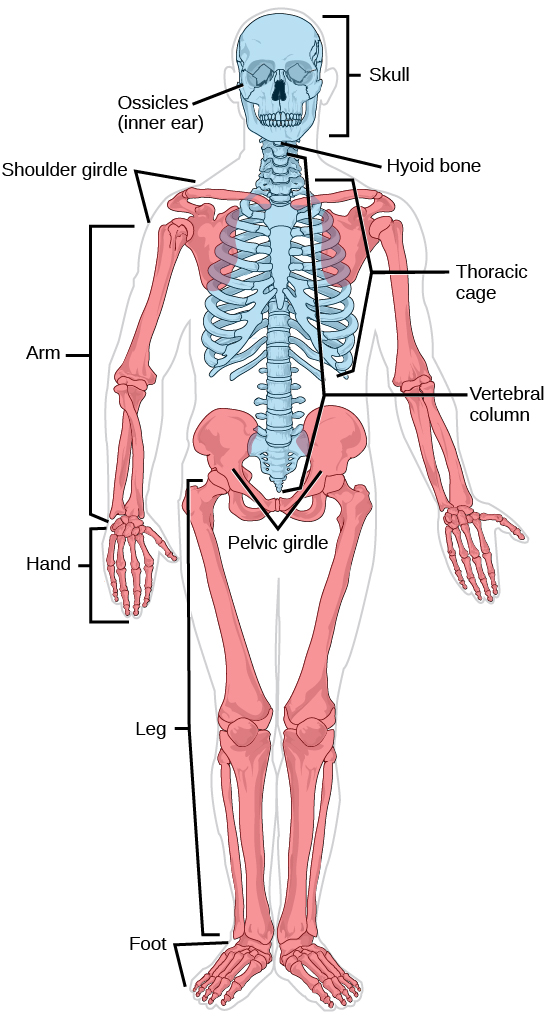
The axial skeleton forms the central axis of the body and includes the bones of the skull, ossicles of the middle ear, hyoid bone of the throat, vertebral column, and the thoracic cage (rib cage) (Figure 11.25).
The bones of the skull support the structures of the face and protect the brain. The skull consists of cranial bones and facial bones. The cranial bones form the cranial cavity, which encloses the brain and serves as an attachment site for muscles of the head and neck. In the adult they are tightly jointed with connective tissue and adjoining bones do not move.
The auditory ossicles of the middle ear transmit sounds from the air as vibrations to the fluid-filled cochlea. The auditory ossicles consist of two malleus (hammer) bones, two incus (anvil) bones, and two stapes (stirrups), one on each side. Facial bones provide cavities for the sense organs (eyes, mouth, and nose), and serve as attachment points for facial muscles.
The hyoid bone lies below the mandible in the front of the neck. It acts as a movable base for the tongue and is connected to muscles of the jaw, larynx, and tongue. The mandible forms a joint with the base of the skull. The mandible controls the opening to the mouth and hence, the airway and gut.
The vertebral column, or spinal column, surrounds and protects the spinal cord, supports the head, and acts as an attachment point for ribs and muscles of the back and neck. It consists of 26 bones: the 24 vertebrae, the sacrum, and the coccyx. Each vertebral body has a large hole in the center through which the spinal cord passes down to the level of the first lumbar vertebra. Below this level, the hole contains spinal nerves which exit between the vertebrae. There is a notch on each side of the hole through which the spinal nerves, can exit from the spinal cord to serve different regions of the body. The vertebral column is approximately 70 cm (28 in) in adults and is curved, which can be seen from a side view.
Intervertebral discs composed of fibrous cartilage lie between adjacent vertebrae from the second cervical vertebra to the sacrum. Each disc helps form a slightly moveable joint and acts as a cushion to absorb shocks from movements such as walking and running.
The thoracic cage, also known as the rib cage consists of the ribs, sternum, thoracic vertebrae, and costal cartilages. The thoracic cage encloses and protects the organs of the thoracic cavity including the heart and lungs. It also provides support for the shoulder girdles and upper limbs and serves as the attachment point for the diaphragm, muscles of the back, chest, neck, and shoulders. Changes in the volume of the thorax enable breathing. The sternum, or breastbone, is a long flat bone located at the anterior of the chest. Like the skull, it is formed from many bones in the embryo, which fuse in the adult. The ribs are 12 pairs of long curved bones that attach to the thoracic vertebrae and curve toward the front of the body, forming the ribcage. Costal cartilages connect the anterior ends of most ribs to the sternum.
The appendicular skeleton is composed of the bones of the upper and lower limbs. It also includes the pectoral, or shoulder girdle, which attaches the upper limbs to the body, and the pelvic girdle, which attaches the lower limbs to the body (Figure 11.25).
The pectoral girdle bones transfer force generated by muscles acting on the upper limb to the thorax. It consists of the clavicles (or collarbones) in the anterior, and the scapulae (or shoulder blades) in the posterior.
The upper limb contains bones of the arm (shoulder to elbow), the forearm, and the hand. The humerus is the largest and longest bone of the upper limb. It forms a joint with the shoulder and with the forearm at the elbow. The forearm extends from the elbow to the wrist and consists of two bones. The hand includes the bones of the wrist, the palm, and the bones of the fingers.
The pelvic girdle attaches to the lower limbs of the axial skeleton. Since it is responsible for bearing the weight of the body and for locomotion, the pelvic girdle is securely attached to the axial skeleton by strong ligaments. It also has deep sockets with robust ligaments that securely attach to the femur. The pelvic girdle is mainly composed of two large hip bones. The hip bones join together in the anterior of the body at a joint called the pubic symphysis and with the bones of the sacrum at the posterior of the body.
The lower limb consists of the thigh, the leg, and the foot. The bones of the lower limbs are thicker and stronger than the bones of the upper limbs to support the entire weight of the body and the forces from locomotion. The femur, or thighbone, is the longest, heaviest, and strongest bone in the body. The femur and pelvis form the hip joint. At its other end, the femur, along with the shinbone and kneecap, form the knee joint.
Joints and Skeletal Movement
The point at which two or more bones meet is called a joint, or articulation. Joints are responsible for movement, such as the movement of limbs, and stability, such as the stability found in the bones of the skull.
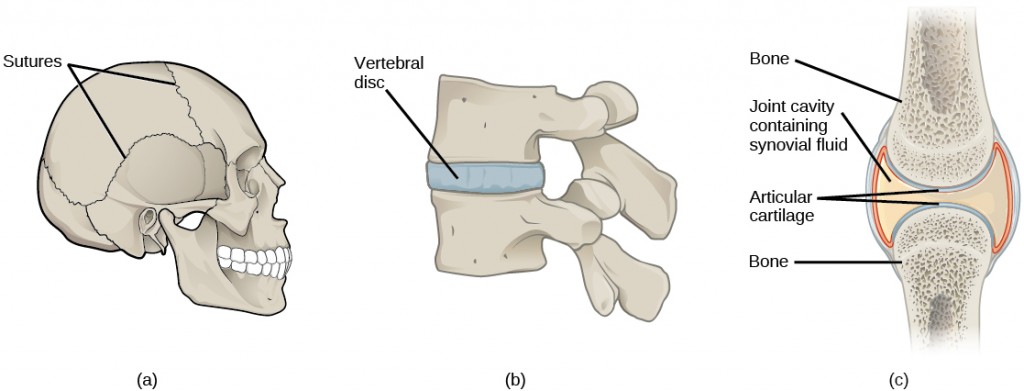
There are two ways to classify joints: based on their structure or based on their function. The structural classification divides joints into fibrous, cartilaginous, and synovial joints depending on the material composing the joint and the presence or absence of a cavity in the joint. The bones of fibrous joints are held together by fibrous connective tissue. There is no cavity, or space, present between the bones, so most fibrous joints do not move at all, or are only capable of minor movements. The joints between the bones in the skull and between the teeth and the bone of their sockets are examples of fibrous joints (Figure 11.26 a).
Cartilaginous joints are joints in which the bones are connected by cartilage (Figure 11.26 b). An example is found at the joints between vertebrae, the so-called “disks” of the backbone. Cartilaginous joints allow for very little movement.
Synovial joints are the only joints that have a space between the adjoining bones (Figure 11.26 c). This space is referred to as the joint cavity and is filled with fluid. The fluid lubricates the joint, reducing friction between the bones and allowing for greater movement. The ends of the bones are covered with cartilage and the entire joint is surrounded by a capsule. Synovial joints are capable of the greatest movement of the joint types. Knees, elbows, and shoulders are examples of synovial joints.
The wide range of movement allowed by synovial joints produces different types of movements. Angular movements are produced when the angle between the bones of a joint changes. Flexion, or bending, occurs when the angle between the bones decreases. Moving the forearm upward at the elbow is an example of flexion. Extension is the opposite of flexion in that the angle between the bones of a joint increases. Rotational movement is the movement of a bone as it rotates around its own longitudinal axis. Movement of the head as in saying “no” is an example of rotation.
Rheumatologist
Rheumatologists are medical doctors who specialize in the diagnosis and treatment of disorders of the joints, muscles, and bones. They diagnose and treat diseases such as arthritis, musculoskeletal disorders, osteoporosis, plus autoimmune diseases like ankylosing spondylitis, a chronic spinal inflammatory disease and rheumatoid arthritis.
Rheumatoid arthritis (RA) is an inflammatory disorder that primarily affects synovial joints of the hands, feet, and cervical spine. Affected joints become swollen, stiff, and painful. Although it is known that RA is an autoimmune disease in which the body’s immune system mistakenly attacks healthy tissue, the exact cause of RA remains unknown. Immune cells from the blood enter joints and the joint capsule causing cartilage breakdown and swelling of the joint lining. Breakdown of cartilage causes bones to rub against each other causing pain. RA is more common in women than men and the age of onset is usually between 40 to 50 years.
Rheumatologists can diagnose RA based on symptoms such as joint inflammation and pain, x-ray and MRI imaging, and blood tests. Arthrography is a type of medical imaging of joints that uses a contrast agent, such as a dye that is opaque to x-rays. This allows the soft tissue structures of joints—such as cartilage, tendons, and ligaments—to be visualized. An arthrogram differs from a regular x-ray by showing the surface of soft tissues lining the joint in addition to joint bones. An arthrogram allows early degenerative changes in joint cartilage to be detected before bones become affected.
There is currently no cure for RA; however, rheumatologists have a number of treatment options available. Treatments are divided into those that reduce the symptoms of the disease and those that reduce the damage to bone and cartilage caused by the disease. Early stages can be treated with rest of the affected joints through the use of a cane, or with joint splints that minimize inflammation. When inflammation has decreased, exercise can be used to strengthen muscles that surround the joint and to maintain joint flexibility. If joint damage is more extensive, medications can be used to relieve pain and decrease inflammation. Anti-inflammatory drugs that may be used include aspirin, topical pain relievers, and corticosteroid injections. Surgery may be required in cases where joint damage is severe. Physicians are now using drugs that reduce the damage to bones and cartilage caused by the disease to slow its development. These drugs are diverse in their mechanisms but they all act to reduce the impact of the autoimmune response, for example by inhibiting the inflammatory response or reducing the number of T lymphocytes, a cell of the immune system.
Muscles
Muscles allow for movement such as walking, and they also facilitate bodily processes such as respiration and digestion. The body contains three types of muscle tissue: skeletal muscle, cardiac muscle, and smooth muscle (Figure 11.27).
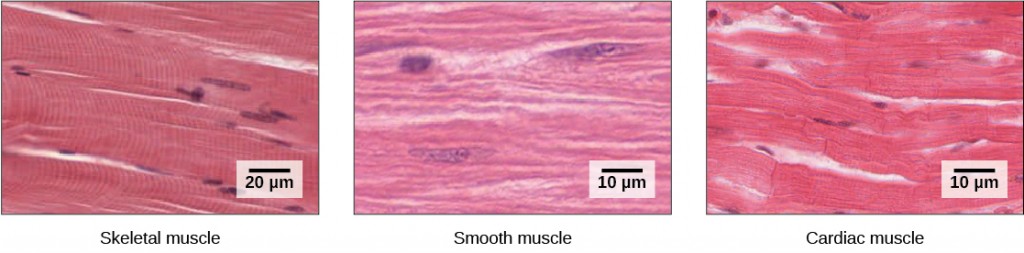
Skeletal muscle tissue forms skeletal muscles, which attach to bones and sometimes the skin and control locomotion and any other movement that can be consciously controlled. Because it can be controlled intentionally, skeletal muscle is also called voluntary muscle. When viewed under a microscope, skeletal muscle tissue has a striped or striated appearance. This appearance results from the arrangement of the proteins inside the cell that are responsible for contraction. The cells of skeletal muscle are long and tapered and have multiple nuclei on the periphery of each cell.
Smooth muscle tissue occurs in the walls of hollow organs such as the intestines, stomach, and urinary bladder, and around passages such as in the respiratory tract and blood vessels. Smooth muscle has no striations, is not under voluntary control, and is called involuntary muscle. Smooth muscle cells have a single nucleus.
Cardiac muscle tissue is only found in the heart. The contractions of cardiac muscle tissue pump blood throughout the body and maintain blood pressure. Like skeletal muscle, cardiac muscle is striated, but unlike skeletal muscle, cardiac muscle cannot be consciously controlled and is called involuntary muscle. The cells of cardiac muscle tissue are connected to each other through intercalated disks and usually have just one nucleus per cell.
Skeletal Muscle Fiber Structure and Function
Each skeletal muscle fiber is a skeletal muscle cell. Within each muscle fiber are myofibrils, long cylindrical structures that lie parallel to the muscle fiber. Myofibrils run the entire length of the muscle fiber. They attach to the plasma membrane, called the sarcolemma, at their ends, so that as myofibrils shorten, the entire muscle cell contracts (Figure 11.28).
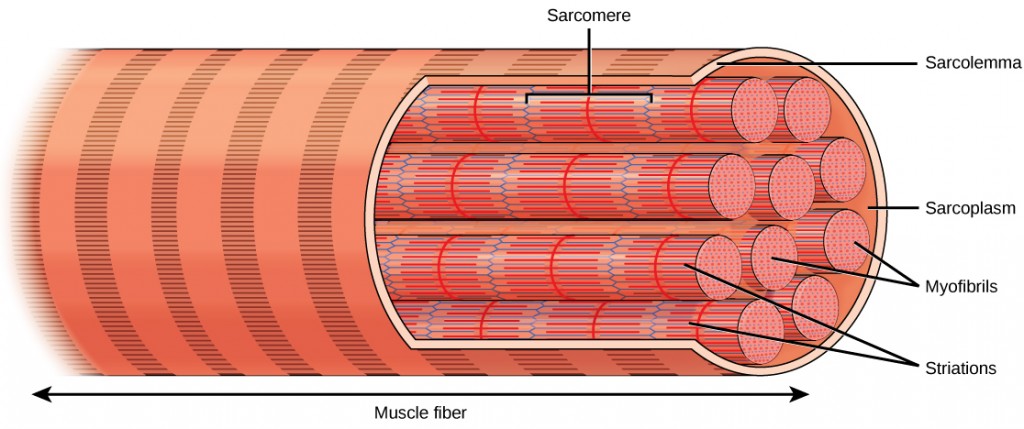
The striated appearance of skeletal muscle tissue is a result of repeating bands of the proteins actin and myosin that occur along the length of myofibrils.
Myofibrils are composed of smaller structures called myofilaments. There are two main types of myofilaments: thick filaments and thin filaments. Thick filaments are composed of the protein myosin. The primary component of thin filaments is the protein actin.
The thick and thin filaments alternate with each other in a structure called a sarcomere. The sarcomere is the unit of contraction in a muscle cell. Contraction is stimulated by an electrochemical signal from a nerve cell associated with the muscle fiber. For a muscle cell to contract, the sarcomere must shorten. However, thick and thin filaments do not shorten. Instead, they slide by one another, causing the sarcomere to shorten while the filaments remain the same length. The sliding is accomplished when a molecular extension of myosin, called the myosin head, temporarily binds to an actin filament next to it and through a change in conformation, bends, dragging the two filaments in opposite directions. The myosin head then releases its actin filament, relaxes, and then repeats the process, dragging the two filaments further along each other. The combined activity of many binding sites and repeated movements within the sarcomere causes it to contract. The coordinated contractions of many sarcomeres in a myofibril leads to contraction of the entire muscle cell and ultimately the muscle itself. The movement of the myosin head requires ATP, which provides the energy for the contraction.
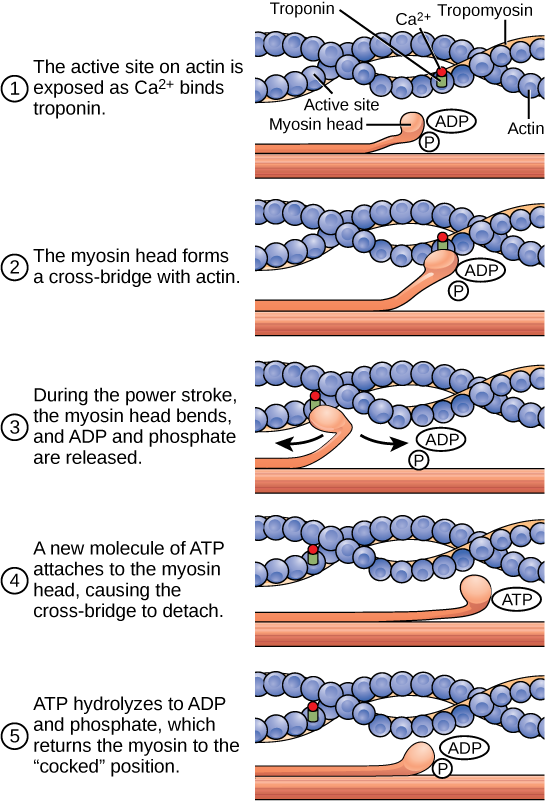
Sliding Filament Model of Contraction
For a muscle cell to contract, the sarcomere must shorten. However, thick and thin filaments—the components of sarcomeres—do not shorten. Instead, they slide by one another, causing the sarcomere to shorten while the filaments remain the same length. The sliding filament theory of muscle contraction was developed to fit the differences observed in the named bands on the sarcomere at different degrees of muscle contraction and relaxation. The mechanism of contraction is the binding of myosin to actin, forming cross-bridges that generate filament movement (Figure 11.29).
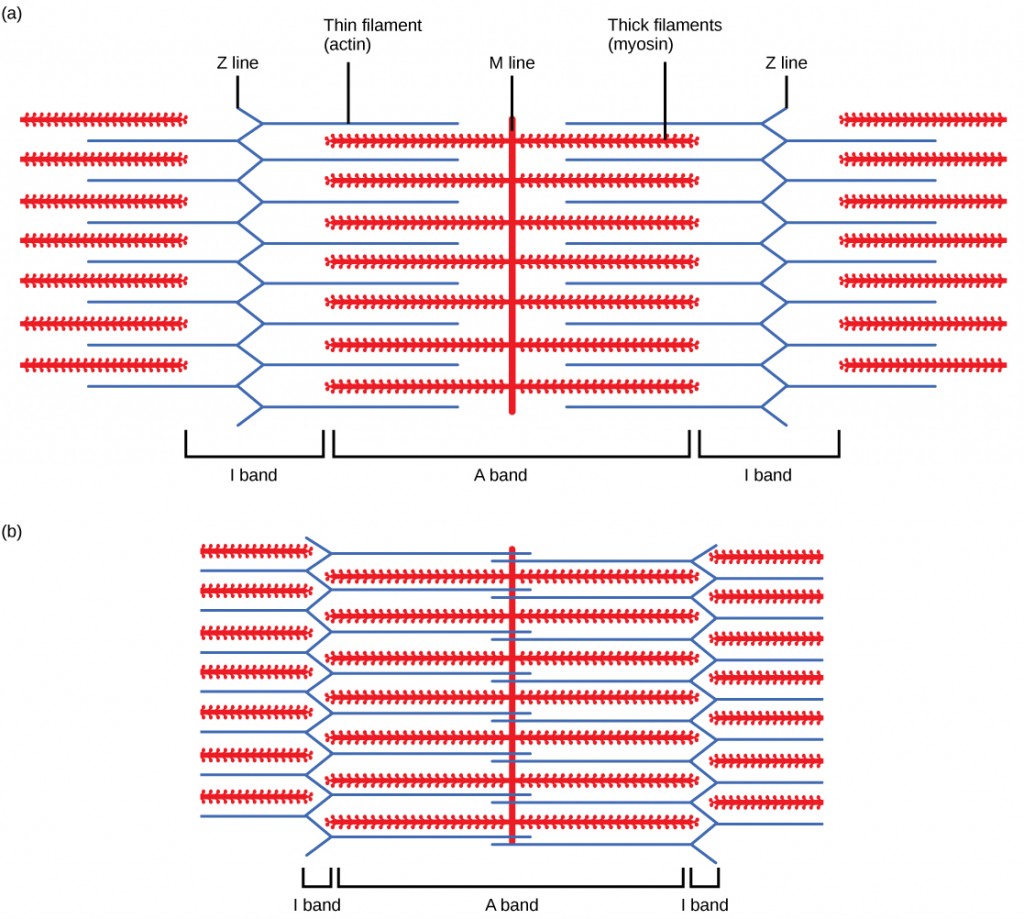
When (a) a sarcomere (b) contracts, the Z lines move closer together and the I band gets smaller. The A band stays the same width and, at full contraction, the thin filaments overlap.
When a sarcomere shortens, some regions shorten whereas others stay the same length. A sarcomere is defined as the distance between two consecutive Z discs or Z lines; when a muscle contracts, the distance between the Z discs is reduced. The H zone—the central region of the A zone—contains only thick filaments and is shortened during contraction. The I band contains only thin filaments and also shortens. The A band does not shorten—it remains the same length—but A bands of different sarcomeres move closer together during contraction, eventually disappearing. Thin filaments are pulled by the thick filaments toward the center of the sarcomere until the Z discs approach the thick filaments. The zone of overlap, in which thin filaments and thick filaments occupy the same area, increases as the thin filaments move inward.
ATP and Muscle Contraction
The motion of muscle shortening occurs as myosin heads bind to actin and pull the actin inwards. This action requires energy, which is provided by ATP. Myosin binds to actin at a binding site on the globular actin protein. Myosin has another binding site for ATP at which enzymatic activity hydrolyzes ATP to ADP, releasing an inorganic phosphate molecule and energy.
ATP binding causes myosin to release actin, allowing actin and myosin to detach from each other. After this happens, the newly bound ATP is converted to ADP and inorganic phosphate, Pi. The enzyme at the binding site on myosin is called ATPase. The energy released during ATP hydrolysis changes the angle of the myosin head into a “cocked” position. The myosin head is then in a position for further movement, possessing potential energy, but ADP and Pi are still attached. If actin binding sites are covered and unavailable, the myosin will remain in the high energy configuration with ATP hydrolyzed, but still attached.
If the actin binding sites are uncovered, a cross-bridge will form; that is, the myosin head spans the distance between the actin and myosin molecules. Pi is then released, allowing myosin to expend the stored energy as a conformational change. The myosin head moves toward the M line, pulling the actin along with it. As the actin is pulled, the filaments move approximately 10 nm toward the M line. This movement is called the power stroke, as it is the step at which force is produced. As the actin is pulled toward the M line, the sarcomere shortens and the muscle contracts.
When the myosin head is “cocked,” it contains energy and is in a high-energy configuration. This energy is expended as the myosin head moves through the power stroke; at the end of the power stroke, the myosin head is in a low-energy position. After the power stroke, ADP is released; however, the cross-bridge formed is still in place, and actin and myosin are bound together. ATP can then attach to myosin, which allows the cross-bridge cycle to start again and further muscle contraction can occur (Figure 11.30).
Concept in Action

Watch this video explaining how a muscle contraction is signaled.
Section Summary
The human skeleton is an endoskeleton that is composed of the axial and appendicular skeleton. The axial skeleton is composed of the bones of the skull, ossicles of the ear, hyoid bone, vertebral column, and ribcage. The skull consists of eight cranial bones and 14 facial bones. Six bones make up the ossicles of the middle ear, while the hyoid bone is located in the neck under the mandible. The vertebral column contains 26 bones and surrounds and protects the spinal cord. The thoracic cage consists of the sternum, ribs, thoracic vertebrae, and costal cartilages. The appendicular skeleton is made up of the upper and lower limbs. The pectoral girdle is composed of the clavicles and the scapulae. The upper limb contains 30 bones in the arm, the forearm, and the hand. The pelvic girdle attaches the lower limbs to the axial skeleton. The lower limb includes the bones of the thigh, the leg, and the foot.
The structural classification of joints divides them into fibrous, cartilaginous, and synovial joints. The bones of fibrous joints are held together by fibrous connective tissue. Cartilaginous joints are joints in which the bones are connected by cartilage. Synovial joints are joints that have a space between the adjoining bones. The movement of synovial joints includes angular and rotational. Angular movements are produced when the angle between the bones of a joint changes. Rotational movement is the movement of a bone as it rotates around its own longitudinal axis.
The body contains three types of muscle tissue: skeletal muscle, cardiac muscle, and smooth muscle. Muscles are composed of individual cells called muscle fibers. Muscle fibers consist of myofilaments composed of the proteins actin and myosin arranged in units called sarcomeres. Contraction of the muscle occurs by the combined action of myosin and actin fibers sliding past each other when the myosin heads bind to the actin fiber, bend, disengage, and then repeat the process.