Chapter 6. States of Consciousness
Drugs and Altered Consciousness
Jessica Motherwell McFarlane
Approximate reading time: 80 minutes
Content Disclosure and Reader Advisory
This section contains discussions on the psychological and physiological impacts of drug use, including detailed information on drug side effects, overdose, addiction, and treatment. It covers a range of substances and includes descriptions of addiction, withdrawal, and the potential for life-threatening situations, which may be distressing or triggering for some readers. The content is presented with a trauma-informed approach and includes both scientific terminology and plain language explanations. Please consider your comfort level with these topics before reading.
Everyone regularly experiences different states of consciousness, especially during sleep. However, some people also use substances, like drugs, that change their state of consciousness. Some use these substances primarily for their medical benefits, despite knowing they can also alter consciousness. Others deliberately use them to achieve a change in their mental state. In this section, we’ll explore various psychoactive drugs—substances that affect the mind—and discuss their therapeutic and side effects on both our physical health and mental states. We’ll look at how these drugs influence our bodies and minds, providing insights into their broader impacts.
Drug Effects and Side Effects
Let’s begin by defining some scientific terms for various drug effects.
Drug Effects Glossary
Psychoactive drugs exert significant effects on the body, affecting both physical and psychological functions. To understand these effects comprehensively, it’s essential to define key terms related to drug use, such as drug withdrawal, drug dependency, and tolerance.
Reuptake is like the brain’s way of recycling unused neurotransmitters. After brain cells send signals to each other with chemicals called neurotransmitters, reuptake is the process of these chemicals being pulled back into the original cell. This stops the signal and gets the cell ready to send the next message. It’s like ending one conversation before starting another.
An agonist is like a key that fits into a lock (which in this case is a receptor in the body). When the key turns the lock, it activates the receptor, causing a specific action or effect in the body. For example, if the lock controls a door that releases happiness (like the release of a feel-good chemical in the brain), turning the key with an agonist opens the door and makes you feel happy.
An antagonist, on the other hand, also fits into the lock but doesn’t turn it. Instead, it blocks the lock so that the usual key can’t open the door anymore. This stops normal action from happening. If we use the same door analogy, an antagonist would prevent the door that releases happiness from being opened, no matter how many times the usual key tries to turn it. This can stop or reduce a specific action or effect in the body that would normally occur.
Study Hint
If it’s an agonist, think of it amplifying (👍).
If it’s an antagonist, think of it opposing and blocking (🚫).
Physical Dependence refers to the body’s adaptation to a drug, leading to changes in normal bodily functions. When the drug use is reduced or stopped, individuals experience withdrawal symptoms due to the body’s reliance on the substance for maintaining normal function.
Psychological Dependence is characterised by an emotional or mental need for the drug, which people frequently use to relieve psychological distress. Unlike physical dependence, psychological dependence focuses on the mental craving for the substance, which can be just as compelling and difficult to overcome.
Drug Withdrawal encompasses a range of negative symptoms that occur when a person stops using a drug after becoming physically dependent on it. These symptoms are typically the opposite of the drug’s effects. For instance, withdrawal from sedatives can result in increased arousal and agitation, highlighting the body’s adjusted state to the presence of the drug.
Tolerance develops as a result of physiological dependence, where the individual requires increasingly larger doses of the drug to achieve the same effects they once obtained with smaller amounts. This escalation can lead to dangerous levels of consumption, risking overdose and death.
It’s important to remember that tolerance and withdrawal symptoms can occur even with drugs that are not abused, indicating that physical dependence alone does not necessarily equate to a substance use disorder. The inclusion of psychological dependence, or drug craving, in the diagnostic criteria for Substance Use Disorder in the DSM-5 underscores the complexity of diagnosing and understanding substance-related issues.
Drug Categories
Psychoactive drugs interact with the body’s neurotransmitter systems in complex ways, leading to various effects on consciousness and physiological states. This section categorises these drugs based on their interactions with our neurotransmitter systems, as detailed in Table SC.3. Understanding the role of agonists and antagonists is crucial here.
| Class of Drug | Examples | Effects on the Body | Effects When Used | Psychologically Addicting? |
|---|---|---|---|---|
| Stimulants | Cocaine, amphetamines (including some ADHD medications such as Adderall), methamphetamines, MDMA (“Ecstasy” or “Molly”) | Increased heart rate, blood pressure, body temperature | Increased alertness, mild euphoria, decreased appetite in low doses. High doses increase agitation, paranoia, can cause hallucinations. Some can cause heightened sensitivity to physical stimuli. High doses of MDMA can cause brain toxicity and death. | Yes |
| Sedative-Hypnotics (“Depressants”) | Alcohol, barbiturates (e.g., secobarbital, pentobarbital), Benzodiazepines (e.g., Xanax) | Decreased heart rate, blood pressure | Low doses increase relaxation, decrease inhibitions. High doses can induce sleep, cause motor disturbance, memory loss, decreased respiratory function, and death. | Yes |
| Opiates | Opium, Heroin, Fentanyl, Morphine, Oxycodone, Vicoden, methadone, and other prescription pain relievers | Decreased pain, pupil dilation, decreased gut motility, decreased respiratory function | Pain relief, euphoria, sleepiness. High doses can cause death due to respiratory depression. | Yes |
| Hallucinogens | Marijuana, LSD, Peyote, mescaline, DMT, dissociative anaesthetics including ketamine and PCP | Increased heart rate and blood pressure that may dissipate over time | Mild to intense perceptual changes with high variability in effects based on strain, method of ingestion, and individual differences | Yes |
Watch this video: Tricky Topics: Drug Mechanisms (20.5 minutes)
“Tricky Topics: Drug Mechanisms” video by FirstYearPsych Dalhousie is licensed under the Standard YouTube licence.
Drug Safety Ratio
When it comes to medication, knowing how much is helpful versus how much is harmful is crucial. This is where the concept of a drug safety ratio comes into play. Also known as a “therapeutic index” or “safety margin,” this ratio helps gauge a drug’s safety by comparing the effective dose to the potentially harmful dose. Think of it as a balance scale: on one side is the dose you need to feel better (effective dose), and on the other side is the dose that could cause side effects or harm (harmful dose). A high safety ratio indicates a wide gap between these doses, suggesting the drug is generally safer because there’s a lower risk of overdose. For instance, cannabis has a very high safety ratio of over 1000. Conversely, a low safety ratio, like alcohol’s 10, means there’s a smaller buffer, requiring more caution in dosing.
Here’s a quick look at the safety ratios for various drugs. It’s important to understand that “safer” in this context doesn’t equate to being completely “safe.” Even drugs with high safety ratios can be risky if misused or allowed to interact with other substances, or if an individual has specific health conditions that make them more susceptible to side effects. In addition, some drugs with a relatively high safety ratio may have a higher risk for different genders or ages. That is, what is relatively safe for one gender or age may not be as safe for another. For example, there is evidence that cannabis use disorder in some young men, more so than in women, is linked to schizophrenia (National Institute on Drug Abuse, 2023b). Therefore, while a high safety ratio can provide some reassurance about the relative risk of overdose or adverse effects, it does not eliminate the need for cautious and informed use of the drug.
According to Gable RS. (2004), here are the safety ratios for some of the more commonly used drugs.
| Drug | Safety Ratio (the bigger the ratio, the safer the drug. Note “safer “does not mean “safe”) |
|---|---|
| Cannabis | >1000 |
| Psilocybin | 1000 |
| LSD | 1000 |
| Prozac | 100 |
| Ketamine | 38 |
| Codeine | 20 |
| Methadone | 20 |
| MDMA | 16 |
| Cocaine | 16 |
| Alcohol | 10 |
| Methamphetamine | 10 |
| GHB | 8 |
| Heroine | 6 |
Depressants
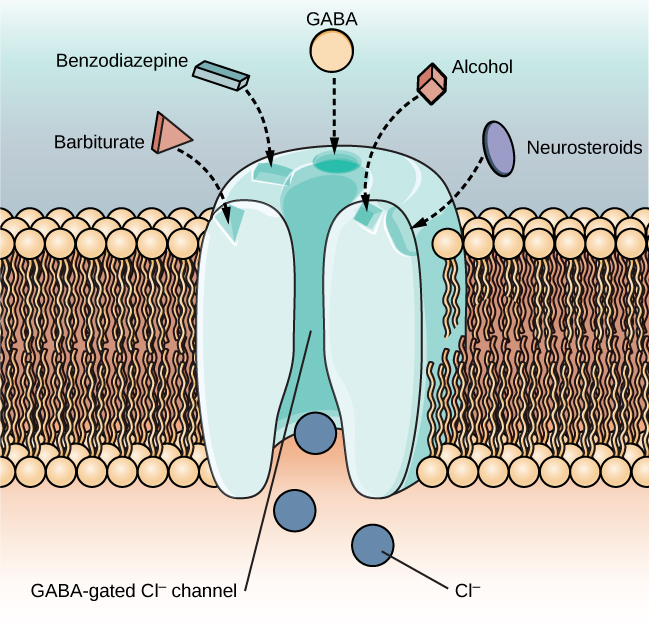
A depressant is a drug that tends to suppress central nervous system activity (Figure SC.17). Some depressants include alcohol, barbiturates, and benzodiazepines. These drugs share their ability to serve as agonists of the gamma-Aminobutyric acid (GABA) neurotransmitter system. Because GABA has a quieting effect on the brain, GABA agonists also have a quieting effect; these types of drugs are often prescribed to treat both anxiety and insomnia.
An illustration of a GABA-gated chloride channel in a cell membrane shows receptor sites for barbiturate, benzodiazepine, GABA, alcohol, and neurosteroids, as well as three negatively-charged chloride ions passing through the channel. Each drug type has a specific shape, such as triangular, rectangular or square, which corresponds to a similarly shaped receptor spot.
Alcohol (Ethanol)
Ethanol, which we commonly refer to as alcohol, is in a class of psychoactive drugs known as depressants. Alcohol (ethanol) consumption results in a variety of changes to consciousness. At rather low doses, alcohol use is associated with feelings of euphoria. As the dose increases, people report feeling sedated. Generally, alcohol is associated with decreases in reaction time and visual acuity, lowered levels of alertness, and reduction in behavioural control. With excessive alcohol use, a person might experience a complete loss of consciousness and/or difficulty remembering events that occurred during a period of intoxication (McKim & Hancock, 2013). In addition, if a pregnant person consumes alcohol, the infant may be born with a cluster of birth defects and symptoms collectively called fetal alcohol spectrum disorder (FASD) or fetal alcohol syndrome (FAS). With repeated use of many central nervous system depressants, such as alcohol, a person becomes physically dependent upon the substance and will exhibit signs of both tolerance and withdrawal. Psychological dependence on these drugs is also possible. Therefore, the abuse potential of central nervous system depressants is relatively high. Drug withdrawal is usually an aversive (very distressing) experience, and it can be a life-threatening process in individuals who have a long history of very high doses of alcohol and/or barbiturates. This is of such concern that people who are trying to overcome addiction to these substances should only do so under medical supervision.
On a global scale, alcohol is often ranked high among the most lethal drugs. A study published in The Lancet ranked alcohol as more harmful than heroin and crack cocaine when considering both the harm to the individual and to others. This ranking is based on a comprehensive analysis of the physical, psychological, and social harms caused by these substances (Nutt, King, Saulsbury, & Blakemore, 2010).
Barbiturates and Benzodiazepines
These drugs, also depressants, are often prescribed for anxiety and insomnia. They work by enhancing the quieting effect of GABA. However, with prolonged use, individuals can develop physical and psychological dependence, making withdrawal potentially dangerous and necessitating medical supervision (McKim & Hancock, 2013).
In summary, depressants and stimulants affect neurotransmitters in the brain, leading to their respective calming or stimulating effects. Understanding their mechanisms and impacts is crucial for safe use and effective treatment of related disorders.
Cannabis: THC and CBD
Cannabis, often called marijuana, includes several chemicals that impact both the brain and body. The most notable are THC (tetrahydrocannabinol) and CBD (cannabidiol).
- THC (Tetrahydrocannabinol): THC is what makes people feel “high” when they use marijuana. It works by attaching to specific parts of brain cells called cannabinoid receptors, which are involved in mood, memory, and how we feel pain. When THC activates these receptors, it can change how we perceive things, our mood, and even our thinking processes. This can lead to feelings of happiness, a distorted sense of time, and increased hunger (Volkow et al., 2014).
- CBD (Cannabidiol): CBD is different from THC because it doesn’t cause a high. It’s known for its potential health benefits. CBD might affect the brain’s cannabinoid system in a less direct way than THC, which could be why it can help with pain, anxiety, and inflammation without making people feel intoxicated (Iffland & Grotenhermen, 2017).
- Biological and Psychological Differences: On a biological level, THC and CBD affect the brain’s cannabinoid receptors differently. THC directly triggers these receptors, leading to its mind-altering effects. CBD, however, might work more indirectly or on other body systems, which is why it can have health benefits without the high. Psychologically, THC can impact thinking and mood, sometimes causing short-term memory problems, poor judgment, or even anxiety or paranoia in some cases. CBD, on the other hand, is being researched for its potential to help with mental health issues like anxiety and depression, without the mind-altering effects of THC (Blessing et al., 2015).
- Cannabis on the Lethal Drug Scale: Compared to drugs like opioids or alcohol, cannabis is generally seen as less dangerous in terms of overdose risk or addiction. The chance of dying from a cannabis overdose is very low, especially when compared to other substances. In terms of harm to the individual and others, cannabis usually ranks lower on the drug lethality scale than substances like alcohol, heroin, or cocaine (Nutt et al., 2010). (Note: Refer to the section on schizophrenia in the Psychological Disorders chapter to learn about the significant findings linking cannabis use disorder with an increased risk of developing schizophrenia in some young men.)
Stimulants
Stimulants are drugs that tend to increase overall levels of neural activity. Many of these drugs act as agonists of the dopamine neurotransmitter system. Dopamine activity is often associated with reward and craving; therefore, drugs that affect dopamine neurotransmission often have abuse liability. Drugs in this category include cocaine, amphetamines (including methamphetamine), cathinones (i.e., bath salts), MDMA (ecstasy), nicotine, and caffeine. Cocaine can be taken in multiple ways. While many users snort (sniff up the nose) cocaine, intravenous injection and inhalation (smoking) are also common. The freebase version of cocaine, known as crack, is a potent, smokable version of the drug. Like (with the salt removed so it is smokable) many other stimulants, cocaine agonizes the dopamine neurotransmitter system by blocking the reuptake of dopamine in the neuronal synapse.
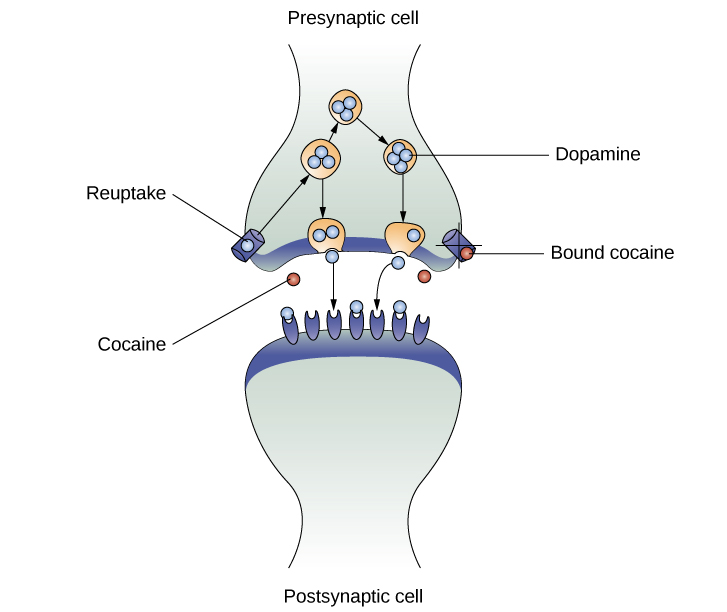
Stimulants are substances that increase neural activity. Many act as agonists of the dopamine neurotransmitter system, which is associated with reward and craving. This category includes drugs like cocaine, amphetamines, methamphetamine, MDMA (ecstasy), nicotine, and caffeine. Cocaine, for example, increases dopamine levels by blocking its reuptake in the neuronal synapse (Jayanthi & Ramamoorthy, 2005; Rothman, Blough, & Baumann, 2007). Cocaine is ranked relatively high on the lethal drug scale due to its potential for overdose and addiction. It poses significant health risks, including cardiovascular problems and neurological effects (Degenhardt & Hall, 2012).
Methamphetamine
Known as “crystal meth,” this highly addictive drug quickly reaches the brain, producing intense euphoria. Its addictive nature leads to prolonged binges, neglecting basic needs like food and sleep. Methamphetamine use can result in severe health issues, including dental problems, skin abrasions, memory loss, and hallucinations (NIDA, 2019). Methamphetamine in its smokable form, often called “crystal meth” due to its resemblance to rock crystal formations, is highly addictive. The smokable form reaches the brain very quickly to produce an intense euphoria that dissipates almost as fast as it arrives, prompting users to continue taking the drug. Users often consume the drug every few hours across days-long binges called “runs,” in which the user forgoes food and sleep.
In the wake of the opiate epidemic, many drug cartels in Mexico are shifting from producing heroin to producing highly potent but inexpensive forms of methamphetamine. The low cost coupled with lower risk of overdose than with opiate drugs is making crystal meth a popular choice among drug users today (NIDA, 2019).
Using crystal meth poses a number of serious long-term health issues, including dental problems (often called “meth mouth”), skin abrasions caused by excessive scratching, memory loss, sleep problems, violent behaviour, paranoia, and hallucinations.
Methamphetamine addiction produces an intense craving that is difficult to treat. In recent years, methamphetamine (meth) use has become increasingly widespread. Methamphetamine is a type of amphetamine that can be made from ingredients that are readily available (e.g., medications containing pseudoephedrine, a compound found in many over-the-counter cold and flu remedies). Despite recent changes in laws designed to make obtaining pseudoephedrine more difficult, methamphetamine continues to be an easily accessible and relatively inexpensive drug option (Shukla, Crump, & Chrisco, 2012).
Methamphetamine is also ranked high on the lethal drug scale. Its addictive nature and the severe health consequences associated with its use, such as cardiovascular and neurological damage, make it a particularly dangerous drug (NIDA, 2019).
Amphetamines
Similar to cocaine, amphetamines block dopamine reuptake and stimulate its release. While they are often abused, they are also prescribed for ADHD, because they increase neurotransmitter activity in brain areas associated with impulse control (Jayanthi & Ramamoorthy, 2005; Rothman, Blough, & Baumann, 2007). That is, by increasing the control of impulse control the ADHD prescribed drugs help improve cognitive processing and decision making. While prescription amphetamines for ADHD are lower on the scale when used as prescribed, illicit use of amphetamines ranks them higher due to the risks of addiction and adverse health effects (Hart, Marvin, Silver, & Smith, 2012). Amphetamines have a mechanism of action quite similar to cocaine in that they block the reuptake of dopamine in addition to stimulating its release (Figure SC.16). While amphetamines are often abused, they are also commonly prescribed to children diagnosed with attention deficit hyperactivity disorder (ADHD). It may seem counterintuitive that stimulant medications are prescribed to treat a disorder that involves hyperactivity, but the therapeutic effect comes from increases in neurotransmitter activity within certain areas of the brain associated with impulse control. These brain areas include the prefrontal cortex and basal ganglia.
MDMA
MDMA (3,4-methelynedioxy-methamphetamine, commonly known as “ecstasy” or “Molly”) is a mild stimulant with perception-altering effects. It is typically consumed in pill form. Users experience increased energy, feelings of pleasure, and emotional warmth. Repeated use of these stimulants can have significant adverse consequences. Users can experience physical symptoms that include nausea, elevated blood pressure, and increased heart rate. In addition, these drugs can cause feelings of anxiety, hallucinations, and paranoia (Fiorentini et al., 2011). Normal brain functioning is altered after repeated use of these drugs. MDMA (Ecstasy/Molly): MDMA is considered to have a moderate risk on the lethal drug scale. While it has a lower risk of fatal overdose compared to drugs like heroin or methamphetamine, it still poses significant health risks, particularly in unregulated settings (Parrott, 2013).
Caffeine
Caffeine, the most widely consumed stimulant worldwide, is present in a variety of beverages, foods, medications, and cosmetics. Its primary pharmacological effect is to antagonise adenosine receptors, thereby inhibiting the action of adenosine, a neurotransmitter that promotes sleep and relaxation. This action of caffeine results in increased alertness and arousal, making it a popular choice for individuals seeking to maintain high levels of wakefulness (Herman & Herman, 2013; Porkka-Heiskanen, 2011).
Despite its benefits, excessive intake of caffeine can lead to adverse health effects, including insomnia, agitation, muscle twitching, nausea, irregular heartbeat, and in extreme cases, death (Reissig, Strain, & Griffiths, 2009; Wolt, Ganetsky, & Babu, 2012). While caffeine’s impact on dopamine neurotransmission is considered indirect, its role as an adenosine antagonist highlights its significant influence on sleep and wakefulness mechanisms (Porkka-Heiskanen, 2011).
Given its widespread availability in medicines, particularly those aimed at weight loss, and its incorporation into various consumer products, understanding caffeine’s pharmacological actions and potential risks is crucial for safe consumption (Herman & Herman, 2013).
The most widely used stimulant, caffeine, found in many beverages and medications, primarily acts by antagonising adenosine activity, promoting wakefulness. High caffeine levels can cause insomnia and other health issues (Herman & Herman, 2013; Porkka-Heiskanen, 2011; Reissig, Strain, & Griffiths, 2009; Wolt, Ganetsky, & Babu, 2012).
Caffeine’s primary biological mechanism of action in the body involves its interaction with adenosine receptors. Adenosine is a neurotransmitter that plays a key role in promoting sleep and suppressing arousal. Under normal circumstances, adenosine accumulates in the brain during waking hours, binding to its receptors and leading to feelings of drowsiness as the day progresses.
When caffeine is consumed, it acts as an adenosine antagonist, meaning it binds to the adenosine receptors without activating them. This prevents adenosine from attaching to its receptors and exerting its sleep-promoting effects. As a result, the natural sleepiness that would occur from adenosine’s action is blocked, leading to increased alertness and wakefulness.
Furthermore, caffeine’s blockade of adenosine receptors indirectly influences other neurotransmitter systems, including the dopaminergic and noradrenergic systems. By inhibiting adenosine’s action, caffeine allows for increased activity of these neurotransmitters, which further contributes to arousal, alertness, and can even enhance mood. These complex interactions of neurotransmitter systems underlies the stimulant effects of caffeine and explains its widespread use as an aid to counteract fatigue and enhance mental performance.
Caffeine is low on the lethal drug scale. While it is widely used and has some mild addictive properties, the health risks associated with caffeine are generally less severe than those associated with other substances listed here (Reissig, Strain, & Griffiths, 2009).
Nicotine
Nicotine is highly addictive, and the use of tobacco products is associated with increased risks of heart disease, stroke, and a variety of cancers. Nicotine exerts its effects through its interaction with acetylcholine receptors. Acetylcholine functions as a neurotransmitter in motor neurons. In the central nervous system, it plays a role in arousal and reward mechanisms.
Nicotine is most commonly used in the form of tobacco products like cigarettes or chewing tobacco; therefore, there is a tremendous interest in developing effective smoking cessation techniques. To date, people have used a variety of nicotine replacement therapies in addition to various psychotherapeutic options in an attempt to discontinue their use of tobacco products.
In general, smoking cessation programs may be effective in the short term, but it is unclear whether these effects persist (Cropley, Theadom, Pravettoni, & Webb, 2008; Levitt, Shaw, Wong, & Kaczorowski, 2007; Smedslund, Fisher, Boles, & Lichtenstein, 2004). Vaping as a means to deliver nicotine is becoming increasingly popular, especially among teens and young adults. Vaping uses battery-powered devices, sometimes called e-cigarettes, that deliver liquid nicotine and flavourings as a vapour. Originally reported as a safe alternative to the known cancer-causing agents found in cigarettes, vaping is now known to be very dangerous and has led to serious lung disease and death in users.
Nicotine, particularly in the form of tobacco products, is high on the lethal drug scale due to its strong addictive properties and the well-documented health risks, including cancer, heart disease, and stroke (U.S. Department of Health and Human Services, 2014).
Opioids and the Opioid Crisis
In our bodies, there’s a natural system designed to manage pain and boost feelings of pleasure. This system produces its own opioid-like substances in small amounts. These substances work by attaching to special areas in the brain known as opioid receptors, helping to lessen pain and create a sense of happiness or euphoria (Pasternak & Pan, 2013). This is why drugs classified as opioids, which are designed to imitate this natural pain relief process, can be highly addictive.

Opioids derived from the opium poppy plant are called opiates. Besides these plant-based opiates, there are also human-made (synthetic) opioids. Opioids are a type of pain relief medication that include drugs like heroin, morphine, methadone, codeine, and oxycodone. These synthetic drugs are very effective at relieving pain but, like their plant-based counterparts, can be misused and lead to addiction due to their strong effects.
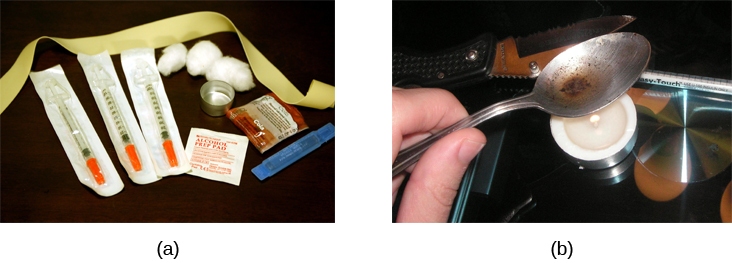
Heroin, for example, can be snorted, smoked, or injected intravenously. Heroin produces intense feelings of euphoria and pleasure, which are amplified when the heroin is injected intravenously. Following the initial “rush,” users experience 4–6 hours of “going on the nod,” alternating between conscious and semiconscious states. Heroin users often shoot the drug directly into their veins; some people who have injected many times into their arms will show “track marks,” while other users will inject into areas between their fingers or between their toes, so as not to show obvious track marks. People who use intravenous drugs have an increased risk of contracting both tuberculosis and HIV.
Opioid use can be risky as it may lead to dependence (a physical need for the drug) and overdose (taking too much of the drug, which can be fatal). Over time, the body can get used to opioids and require more to get the same effect, a situation known as tolerance. Misusing opioids can lead to opioid use disorder, a medical condition involving the inability to stop using the drug despite harmful consequences.
The Rise of the Opioid Crisis
The opioid crisis, particularly severe in North America, began in the 1990s with the over-prescription of opioid pain relievers like OxyContin. These drugs were incorrectly marketed as non-addictive, leading to widespread use and addiction (Canadian Centre on Substance Use and Addiction, 2019; CIHI, 2020; Van Zee, 2009). (The crisis has led to a significant increase in opioid-related deaths, especially in Canada and the United States. For instance, in Canada, more than 3,800 opioid-related deaths were reported in 2019 alone, a 26% increase from the previous year (Public Health Agency of Canada, 2020).
Impact of the Crisis
The opioid crisis has had a devastating impact, particularly in British Columbia (BC), Canada. From 2016 to 2018, BC experienced a dramatic increase in opioid-related overdose deaths, with fentanyl, a very potent synthetic opioid, involved in many cases (Kestler et al., 2019; Krausz et al., 2020). The crisis has affected people of all ages, including young people and children.
Public Health Responses and Naloxone
In response to the crisis, public health initiatives have focused on treatment, recovery services, and the use of Naloxone, an opioid antagonist. Naloxone is a medication that can quickly reverse the effects of an opioid overdose. It works by blocking the opioids from acting on the brain (McDonald & Strang, 2016). (Note: It may take several doses of Naloxone to reverse an opiate overdose.) Programs like the British Columbia Take Home Naloxone (BCTHN) have been effective in reversing overdoses and saving lives (Banjo et al., 2014; Irvine et al., 2019; Young et al., 2019; Karamouzian et al., 2019; Deonarine et al., 2016).
You can train to deliver life-saving Nalaxone
Anyone can train to use naloxone kits; the training is easy, readily available online. Nalaxone will not cause harm if a person hasn’t taken opioids. The kits can be picked up at your local pharmacy.
Will you take the Naloxone training and get a Naloxone kit? You just might save a life.
Watch this video: What causes opioid addiction, and why is it so tough to combat? – Mike Davis (8.5 minutes)
“What causes opioid addiction, and why is it so tough to combat? – Mike Davis” video by TED-Ed is licensed under the Standard YouTube licence.
Hallucinogens and Their Psychological Effects
Hallucinogens are a group of substances that can significantly alter perception, mood, and thought processes. Drugs like LSD, Psilocybin, and DMT mainly affect the brain’s serotonin system, leading to vivid visual hallucinations, changes in thought, and feelings of deep insight. These experiences can range from enlightening to disorienting, with users reporting everything from intense emotional swings to a distorted sense of time. Other hallucinogens, such as PCP and ketamine, interact with different brain receptors, resulting in effects like dissociation, where users feel detached from their bodies or reality. This can be therapeutic but also confusing or disorienting.
Hallucinogens work by interacting with the brain’s serotonin system, particularly affecting receptors that influence mood and perception. When substances like LSD, Psilocybin, and DMT bind to these receptors, they alter the normal functioning of brain cells, leading to changes in consciousness. This can result in vivid visual hallucinations, altered thought processes, and a sense of deep insight or spiritual experience. Beyond serotonin, these drugs can also impact other neurotransmitters like dopamine and glutamate, further influencing emotions and how different parts of the brain communicate with each other. This complex interaction between hallucinogens and the brain’s chemistry is what leads to their powerful and varied effects on the mind.
In addition to their recreational use, some hallucinogens have a long history in Indigenous medicine for spiritual and healing purposes, guided by strict cultural practices. Recently, there’s growing interest in the potential of substances like psilocybin and ketamine as treatments for mental health disorders, including depression and PTSD. Ketamine, for example, has been found to quickly reduce symptoms of severe depression. This shift towards exploring the therapeutic benefits of hallucinogens marks a significant change in how these drugs are viewed in psychology and medicine.
Hallucinogens in Indigenous Medicine
Purpose and Use
- Cultural and Spiritual Significance: In many Indigenous cultures, hallucinogens have been used for centuries for spiritual, medicinal, and ritual purposes. These substances, such as peyote, ayahuasca, and psilocybin mushrooms, are often integral to religious ceremonies and healing practices.
- Healing and Insight: Spiritual leaders or shamans typically guide the indigenous use of hallucinogens, which is believed to facilitate healing, provide spiritual insight, and connect individuals with the natural world and the spiritual realm.
Control and Respect
- Regulated Use: The use of hallucinogens in Indigenous medicine is highly controlled and respected within these cultures. It is not recreational but rather a part of a structured, often sacred practice.
- Integration with Rituals: Skilled practitioners frequently use these substances in specific ritualistic contexts alongside customary songs, prayers, and guidance.
Contemporary Recognition and Challenges
- Legal Recognition: In some regions, the use of certain hallucinogens in Indigenous practices is legally recognised, acknowledging their cultural and spiritual importance. However, this recognition varies by country and region.
- Conservation and Sustainability: The increased interest in these substances poses challenges in terms of conservation and sustainable use, particularly for plants like peyote, which are at risk of over-harvesting.
In psychology, it is crucial to understand the psychological effects of hallucinogens and the therapeutic potential of drugs like ketamine. These substances, once viewed solely as recreational drugs, are now being recognised for their potential in treating complex mental health conditions.
To learn more about some of the most commonly abused drugs, check out the Commonly Abused Drugs Chart and the Commonly Abused Prescription Drugs Chart, both from the National Institute on Drug Abuse.
Watch this video: How Ketamine Treats Depression (5 minutes)
“How Ketamine Treats Depression” video by rainFacts.org is licensed under the Standard YouTube licence.
Watch this video: Altered States: Crash Course Psychology #10 (11 minutes)
“Altered States: Crash Course Psychology #10” video by CrashCourse is licensed under the Standard YouTube licence.
Summary: Drugs and Altered Consciousness
This section explores the complex relationship between drugs and altered states of consciousness, detailing the effects of various substances on the human mind and body. It begins by outlining the general effects drugs can have, including changes in perception, mood, and behaviour. Then we categorise drugs into several groups, providing a detailed table of drugs and their specific effects to give readers a clear understanding of the wide range of available substances and their impact.
We also discuss depressants, such as alcohol, barbiturates, and benzodiazepines, explaining how these substances slow down brain activity and can lead to relaxation or sedation. The section on cannabis focuses on the compounds THC and CBD, highlighting their effects and the ongoing debate surrounding their use. Stimulants, including methamphetamine, amphetamines, MDMA, caffeine, and nicotine, are examined for their ability to increase alertness, energy, and attention, albeit with potential for abuse and addiction.
This section addresses the opioid crisis through an exploration of opioids’ pain-relieving properties and the devastating impact of addiction and overdose, supplemented by a video on the causes of opioid addiction. Hallucinogens are discussed next, with attention to their profound effects on perception and consciousness, including the use of substances like ketamine in treating depression and PTSD, and the role of hallucinogens in indigenous medicine.
Overall, this section covers the diverse effects of drugs on consciousness and mental health, supported by case studies and videos that further explain and illustrate the therapeutic and harmful potentials of these substances.
Image Attributions
Figure SC.17. Figure 4.15 as found in Psychology 2e by OpenStax is licensed under a CC BY 4.0 License.
Figure SC.18. Figure 4.16 as found in Psychology 2e by OpenStax is licensed under a CC BY 4.0 License.
Figure SC.19. Photo by Catalin M is licensed under the Pexels Content License.
Figure SC.20. Figure 4.17 as found in Psychology 2e by OpenStax is licensed under a CC BY 4.0 License and contains modifications of the following work: Needle Exchange by Todd Huffman is licensed under a CC BY 2.0 License.
Figure SC.21. Figure 4.18 as found in Psychology 2e by OpenStax is licensed under a CC BY 4.0 License and contains modifications of the following work: psychedelic curl by new 1lluminati is licensed under a CC BY 2.0 License.
To calculate this time, we used a reading speed of 150 words per minute and then added extra time to account for images and videos. This is just to give you a rough idea of the length of the chapter section. How long it will take you to engage with this chapter will vary greatly depending on all sorts of things (the complexity of the content, your ability to focus, etc).

