17 Health Security in the Context of Social-ecological Change
Chris G. Buse, Donald C. Cole and Margot W. Parkes
Learning Outcomes & Big Ideas
- Demonstrate an understanding of determinants of health, health security and social-ecological systems and the roles they play in supporting health.
- Explicate the inter-relationships between political and economic power, environmental change, and health security in particular places/watersheds/ecosystems/ecoregions through the use of different frameworks and theories. Explain how these dynamics operate at, and across, different scales.
- Illustrate the particular challenges that the diversity, breadth and complexity of health security problems and responses pose to understanding, practice and research. Select and apply different approaches and use a suite of observational and analytic tools to address health security problems.
- Draw on critical understanding of concepts, relationships, and tools as well as their values, motivations and place in the world, to formulate responses (actions, interventions and practice or policy changes) to promote health security. Consider the ways that these may be applied in different professional and organizational settings.
Summary
The focus of this chapter is to demonstrate interlinkages between changing ecological and social systems and health security. Moving beyond dynamics of disease spread and bioterrorism, we draw attention to the reciprocal relationships between living and social systems to exemplify how health security operates at this interface. We clarify key concepts of health, public health, the determinants of health, health security and social-ecological systems, demonstrating their implications for how we understand and respond to health security issues. In doing so, this chapter critically analyzes the health security discourse, and forwards new tools and approaches to expand our understanding of the multiple ways in which health is impacted by changes to ecosystems and resulting social change.
Chapter Overview
17.2 What Are Health and Health Security?
17.2.1 Health and Its Determinants
17.2.2 Health Security: Overview and Challenges
17.3 Coupled Social-ecological Systems and Implications for Health Security
17.3.1 What Are ‘Resilient’ Social-ecological Systems?
17.3.2 Ecological Drivers of Health Insecurity in Coupled Social-ecological Systems
17.3.3 Potential Synergies: Linking Social-ecological Insights with Health Security
17.4 Case Examples Linking Social-ecological Insights with Human Security in Particular Bioregions
17.4.1 Food Security in East Africa
17.4.2 Cumulative Impacts of Multiple Resource Development Operations in Northern British Columbia
17.5.1 Towards Integrative Approaches to Health Security and Social-ecological Change
17.5.2 Recommendations for Future Research, Education and Practice
Extension Activities & Further Research
17.1 Introduction
In an era of rapid social and ecological change, the interfaces of health, human security, and global environmental change warrant particular attention. Accordingly, this chapter foregrounds the notion of health security in relation to social-ecological change. The World Health Organization constitution states that “the health of all peoples is fundamental to the attainment of peace and security and is dependent upon the fullest co-operation of individuals and states” (WHO, 1948, p. 1). Health security therefore exists at the interface of the health and security sectors, and is typically thought of as the activities required to mitigate risk or respond to acute events that endanger population-level health across international boundaries.
This conventional definition of health security therefore privileges concerns of disease outbreaks of epidemic proportions with risks of international transmission, deliberate acts of bioterrorism, and responses to disease in contexts characterized by war or violent conflict. Global health security is arguably more important now than ever before. For example, an influenza pandemic could affect up to 1.5 billion people, be responsible for up to 150 million deaths, and produce USD $3 trillion in economic damages (Hoffman, 2010). While the acute public health and emergency management response is laudable to respond to such direct biophysical threats, one topic that has received limited attention in human and health security discourses is the role of global environmental change.
Leveraging from more traditional definitions of health security, this chapter conceptualizes how global environmental change can impact health security, and builds upon other chapters in this volume that engage with threats to human security (Chapter 5), climate change (Chapter 9), resource scarcity (Chapter 10), human rights (Chapter 15) and global environmental governance (Chapter 20). First, we provide definitions for key terms, highlighting the historical context that led to emergence of health security. Second, we establish the importance of social-ecological systems as an essential component in considering the interface of health security and global environmental change. Third, we profile some of the greatest ecological challenges facing the planet in the 21st century in relation to their implications for health security, and demonstrate the relevance of these challenges through several applied case studies. Finally, we present and discuss the implications of a broader definition of health security, its relationship to globalized equity and ecological considerations, addressing time and scale considerations that span the local to the global, and which point to emerging priorities for public health practice, research and policy moving forward. Our chapter foregrounds essential theoretical and practical considerations to drive future innovation on health security in an era of environmental change. While this chapter is not intended to be an exhaustive review of the concept of health security or the myriad social-ecological challenges facing the human population, we anticipate it will be helpful for audiences from health and non-health sectors in clarifying key terminology, and establishing connections between seemingly unconnected health issues as security challenges.
17.2 What Are Health and Health Security?
This section provides an overview of the concept of health and its determinants to set the stage for an introduction to the concept of health security. We provide an overview of key terminology and discuss the implications of health security in relation to health not only as an outcome, but in terms of its broader determinants.
17.2.1 Health and Its Determinants
Health refers to “a state of complete physical, mental and social well-being, not merely the absence of disease or infirmity” (WHO, 1948, p. 1). Health is therefore both a state, outcome and process that plays out at the level of an individual (i.e. when we get sick or experience an injury), but also at the level of populations. Individual health is typically treated by health professionals across health and social systems of care, whereby health systems are typically considered a front-line response to protecting against disease population health (Kutzin & Sparkes, 2016). Preventative aspects of population-level health are the responsibility of public health — which, as a field of research, policy and practice, has the role of protecting and promoting health, preventing disease and injury, and reducing health inequities. Public health is therefore directly informed by the cross-disciplinary study of, but also practice and policy directed towards, population health and its determinants. Health is not only a product of individual choice and genetics, but is the direct result of social, political, economic and environmental determinants (Marmot 2009). These determinants of health modify and influence who bears the burden of a disease or chronic condition and the extent of the impact on both individuals and populations, and explain group differences in health status (Marmot, 2009; Mikkonen & Raphael, 2010).
Including the determinants of health in a conversation about health security is incredibly important. The determinants of health refer not only to the things which negatively influence our health over time, but also our adaptive capacity to respond to threats. By broadening our understanding of health beyond any single impact to recognize the broader context(s) of ill-health, we are able to connect health and security to questions of livelihoods, geopolitics, social relationships, and ecological systems. For example, a modelling study estimated the cost of a hypothetical infectious disease outbreak to be between $13 million to $64 million for one country, to $8 billion to $41 billion for nine countries, placing between 1500 to 1.4 million export-related jobs at risk (Bambery et al., 2018). Not only does an infectious disease pandemic therefore impact individuals and populations in terms of their health, but it will also affect the systems of care treating those affected, and have massive economic impacts that may slow economic development at best, or threaten economic and regional destabilization at worst, ultimately influencing the security of a population to afford the basic necessities of life (Cameron, 2017). Thus, health in a security context, must necessarily account not only for health-related outcomes, but also the features that determine, modify or mediate those outcomes.
17.2.2 Health Security: Overview and Challenges
According to McInnes (2015, p. 7), there are “… four terms widely used in debates over health security in the global context…global (public) health security, national security, human security and biosecurity” and that they are not synonymous, reflect different interests and agendas, and have different implications for how we understand the health and security nexus (Lo Yuk-ping & Thomas, 2010). National security typically refers to securing the borders of a country and the welfare of the citizens within its bounds. Biosecurity is a field of study intended to protect humans, plants and animals against harmful biological agents, and in some contexts such as New Zealand, has been interpreted to include entire ecosystems. Human security, as outlined throughout this text, and as defined by the United Nations, is an approach for “identifying and addressing widespread and cross-cutting challenges to the survival, livelihood and dignity of their people” (UN General Assembly Resolution 66/290, Article 3, p.1). Related to each of these three concepts is the notion of health security or global public health security which are often used interchangeably.
For example, let us briefly return to the WHO constitutional mandate for achieving health for all through security and peace. In this context, and as articulated by Aldis (2008, p. 370), “’security’ seems to refer to ‘health and security’ (the contribution that health makes to global security) rather than to ‘health security’ (securing health itself).” Importantly, there seem to be no universally agreed upon definitions for health security (Lee & McInnes, 2004; Rushton, 2011). There are, however, several recurrent themes across the health and human security literatures emerging from a published literature review, which include:
- Protection against threats (e.g. disease, poverty, oppression, hunger, etc.)
- Emergence of new global conditions under which past approaches produce diminishing returns (e.g. rise of failed states, emerging environmental threats, etc.)
- Engaging new allies (e.g. public health collaboration with military establishments)
- Linking health to foreign policy interests (e.g. HIV/AIDS pandemic as a national and international security threat).[1]
Following Lee and McInnes (2004), a global health issue can rise to prominence on international security agendas if it is international in scope, threatens economic destabilization, impacts the stability of a region, and/or when health issues are part of trade negotiations. Feldbaum and Lee (2004) similarly highlight that a global health security threat typically impacts populations of people rather than individual health, produces a high incidence of death or disease, produces acute rather than long-term or chronic health impacts, and are experienced by more than one country. Much of the health security literature echoes these criteria, whereby extreme threats of international proportion establish legitimacy for a substantial political response.
Indeed, the discourse of health security dates back centuries as a reflection of historical disease outbreaks, more recently converging around the increasing importance of public health security in a highly globalized world (Kamradt-Scott, 2015; Novotny, 2007). Hoffman (2010) characterizes global health security according to four regimes:
- Unilateral quarantine regulations (1377–2851)
- A series of sanitary conferences beginning in 1851 to develop international agreements around infectious disease response
- The establishment of several international sanitary conventions and international health organizations (1892–1946)
- Under the leadership of the WHO (1946–present).
This last regime which has been challenged by an increasingly globalized and interconnected world, recently culminated in The International Health Regulations (IHR) created by the WHO in 2005 and its member states (Kamradt-Scott, 2011; Katz et al., 2014; Kennedy et al., 2018; Paranjape & Franz, 2015; Wilson et al., 2008). Driven largely by the severe acute respiratory syndrome (SARS) outbreaks in Canada and China, but also increasing concerns over variations in pandemic influenza and heightened security concerns over terrorist activities, the IHR “aim to prevent, protect against, control and provide a public health response to the international spread of disease” (Article 2), with the intent of incorporating “biological, chemical and radio-nuclear events, as all as zoonotic diseases and threats to food safety” (Gostin & Katz, 2016, p. 267).
Thus, health security under the IHR encompasses not only traditional biological threats such as the spread of disease either naturally or otherwise, but also terrorist attacks (Eisenman et al., 2004; Khan, 2011), and nuclear and biological weapons (e.g. engineered pathogens or otherwise) (Carus, 2015; Colf, 2016). Perhaps overlooked elements of health security under the IHR may include human trafficking and other disease transmission pathways (Worsnop, 2019), antimicrobial resistance (Toner et al., 2015), mass migrations (MacPherson et al., 2007; Viettie et al., 2013; Zimmerman et al., 2011), and other so-called global catastrophic biological risks which include climate change and violent conflicts (Barnett & Adger, 2007; Percival & Homer-Dixon, 1998; Schoh-Spana et al., 2017; see also Chapter 5).
These trends reflect an increased focus on global governance in relation to health security, and how security discourses have become a dominant response to global health threats (Chen & Narasimhan, 2003; Fidler, 2007; McInnes, 2005). These developments have arguably led to a privileging of infectious diseases as central issues in the health security discourse (e.g. pandemic influenza, Ebola, HIV/AIDS, Zika), which has engendered a particular emphasis on improving global health surveillance platforms for data sharing, enhancing laboratory testing, workforce development, and promoting rapid humanitarian and emergency response (Balajee et al., 2016; Belay et al., 2017; Borchert et al., 2014; Fitzmaurice et al., 2017; Sikka et al., 2016; Tappero et al., 2017). This necessarily includes building effective systems of care and associated emergency management protocols in order for primary health care to be an effective contributor to health security and associated reactive and proactive responses (Chan, 2009). Indeed, local health departments play significant roles in responding to the immediate and longer-term recovery from health security threats, and require programming to support training, safety, public preparedness, planning for emergency response and evaluation (Errett et al., 2015; Taylor et al., 2018). Moreover, policy frameworks such as the IHR necessarily stress the importance of international collaboration and the need for diplomacy to achieve policy coherence that supports the promotion of health security in a rapidly globalizing world (Bond, 2008; Frieden et al., 2014).
Although these developments in health security bring new perspective through renewed foci on governance, conflict, diplomacy and disease, we find these approaches to health security and associated responses problematic for at least three reasons. First, much of what is outlined above is reactive in nature, rather than proactive in mitigating the risk of the threat to health security in the first place. A second concern is that these approaches to health security do not engage fulsomely or directly with our earlier definitions of health in relation to its broader determinants. A third, interrelated concern, is the growing need to address the converging implications of both social and ecological change for health security.
This last concern in particular has been raised by authors such as Ostergard and Kauneckis (2014) who examine research on climate change impacts to human health security. The overarching concern raised here is that the health security literature has tended to emphasise and exemplify acute events that create health emergencies, but larger, slower-moving emergencies such as global environmental change — which pose significant health threats, but also an existential threat to the human species — have typically been neglected. Instead, health security discourses seem to primarily respond to emergent implications of global environmental change such as changes in the distribution and patterning of disease vectors, or emergency response following extreme climate events (e.g. hurricanes), without adequate attention to preventing the upstream drivers of these threats. In the following sections we seek to rectify this shortcoming by drawing attention to converging social and ecological drivers of change influencing health security, through the fast and slow-moving influences on broader determinants of health.
17.3 Coupled Social-ecological Systems and Implications for Health Security
We now turn our attention to the interface between social and ecological systems and implications for health, acknowledging foundational work with direct relevance to health security, and moving to describe the value of considering health security in relation to social-ecological systems and the discourse of resilience. Some would argue that the Ottawa Charter for Health Promotion (WHO, 1986) offers a precursor to a more integrative approach to health security, with its emphasis that improvements in health required a secure foundation in the basic prerequisites for health, listing these prerequisites as: peace, shelter, education, food, income, a stable ecosystem, sustainable resources, social justice and equity. This emphasis led to the Ottawa Charter’s call for a “socioecological approach” to health, noting:
The inextricable links between people and their environment constitutes the basis for a socioecological approach to health. The overall guiding principle for the world, nations, regions and communities alike is the need to encourage reciprocal maintenance – to take care of each other, our communities and our natural environment. (WHO, 1986, Section 2, Article 2 ‘Create Supportive Environments’, n.p.)
The value of combined social and ecological orientation to health has been echoed and reiterated through subsequent decades of public health efforts. Along with efforts to fulsomely engage with both the ecological and the social determinants of health (see Cole et al., 1999; Edwards & Davison, 2015; Horwitz & Parkes, 2019; McLaren & Hawe, 2005; Parkes et al., 2003), a combined emphasis on the social and ecological determinants of health can be seen across emerging fields of public health research and practice such as ecohealth, environmental health equity, One Health and planetary health (see Buse, Oestreicher et al., 2018). As well as efforts focused on health of humans (and other species), an important concurrent body of work has generated expanding attention to social-ecological systems (SES), change and resilience, and offers a very helpful complement to an integrative understanding of health security. The remainder of this section, provides an overview of the dynamics of coupled social and ecological systems before linking these to the emergent health security dimensions of ecological change, and returning to the benefits of an integrative, social and ecological orientation to health security.
17.3.1 What Are ‘Resilient’ Social-ecological Systems?
SES are complex assemblages of social actors, institutions and bio-geo-physical units, that adapt and respond to shocks or changes based on their composition, function, and spatial and temporal orientations (Berkes et al., 2003; Levin, 1998). In other words, SES refer to the relationships of social systems (i.e. society) to the ecological systems and ecosystem services which provide conditions for life to sustain and flourish (Holling, 2001). Thus, not only are ecosystem processes essential to the functioning of social-ecological systems, but so too are the human relationships, institutions and power dynamics that govern social and ecological systems alike (Cote & Nightingale, 2012; Cretney, 2014; Smith & Stirling, 2010).
SES tend to be nested within multiple hierarchical systems, where smaller systems move rapidly through processes of exploitation, conservation, release and reorganization (Holling, 2001). Holling (1986) famously used the example of forest fires to depict how a forest system would grow, exploiting available resources of oxygen, land and nutrients from the soil, ultimately crowding out other elements and producing competition over resources that requires the forest to ultimately conserve those resources. When triggered under the right conditions, sometimes by an exogenous event such as lightning from a thunder storm, a fire could release the massive amounts of stored energy and potential of the system, ultimately creating opportunities for reorganization into a similar system (e.g. a forest), or into an entirely new system altogether. Termed what Gunderson and Holling refer to as ‘panarchy,’ adaptive SES rely on an ability for systems that operate at different spatial and temporal scales to experiment with novel assemblages at small scales while larger, slower moving systems protect against catastrophic systems change while still benefitting from the innovation, creation and conservation of smaller systems (Gunderson & Holling, 2002; Holling, 2001).
SES rose to prominence primarily when considering the resilience of ecological systems and human communities in relation to natural disasters and resource management issues (Folke, 2006; Gunderson, 2010). SES are often discussed in terms of their resilience, vulnerability and adaptability across time and geographic space (Young, 2014). The resilience approach emphasizes that systems are characterized by non-linear dynamics, thresholds and tipping points for change, uncertainty, and have multiple interactions across time and space (Folke, 2006; Walker et al., 2004). Resilience typically reflects a system’s ability to respond to shocks so as to return to its original function, but has increasingly been recognized that ‘bouncing back’ to a system that is inherently unsustainable may be problematic in the context of SES, and therefore, much conventional scholarship emphasizes the learning of systems and the actors within it and their ability to ‘bounce forward’, learn from shocks and ultimately self-organize to produce a more effective systems response (Berbes-Blasquez et al., 2014). Accordingly, a resilient system is more able to adapt to shocks and could either proactively or reactively respond to systems vulnerabilities to minimize the impacts of the shock across the system or for its specific components. Alongside resilience, a focus on social-ecological change is fuelling necessary attention to understanding processes of transformation in communities and societies (Andrachuk & Armitage, 2015; Chandra et al., 2010; Kull et al., 2018) in ways that are highly relevant to our future health and security.
Recognition of the links among SES resilience, change and the determinants of health is expanding (Berbes-Blasquez et al., 2014; Bunch et al., 2011). Indeed, it has been argued that, within specific SES contexts — for example, catchments and watersheds — that “promotion of health and resilience converge towards a common goal: to cultivate enduring capacity to respond positively to change and challenges” (Parkes & Horwitz, 2009, p. 100). Given that health security will always need to address shocks, change and challenges, we argue that understanding of both resilience and health in SES will be essential if health security is to be understood in a way that actively addresses combined and converging social and ecological change.
17.3.2 Ecological Drivers of Health Insecurity in Coupled Social-ecological Systems
The 21st century has presented dramatic natural and anthropogenic environmental changes that pose unique risks to human health. For example, climate change has raised global temperatures where 17 of the 18 warmest years on record have occurred since the turn of the 21st CE (NASA, 2018). As a result of increasing carbon pollution, ocean acidification threatens all forms of marine life, and in 2015 the Great Barrier Reef experienced the largest single bleaching event to ever occur with deleterious effects on marine biodiversity in that area. Further, the use of non-biodegradable consumer items has led to other forms of ecological marine stress. There are now at least five massive garbage patches across the planet’s oceans comprised almost entirely of microplastics and plastic products. This pollution exists on a previously unimaginable scale, impacting marine life and impacting biodiversity of the ocean. On land, deforestation — the permanent destruction of a forest to make way for other land uses — results in an estimated 18.7 million acres of forest loss every year (WWF, 2018) contributing to approximately 15% of global greenhouse gas emissions. Other forms of large-scale resource ‘development’ (e.g. the construction of hydroelectric dams, mines, fracking natural gas, etc.) also contribute to these trends, while creating massive linear disturbances on the landscape for supporting infrastructure, and often contributing to poor air quality and water contamination.
These changes to marine, terrestrial and atmospheric environments are so great, that geologists maintain we now live in a new geological epoch named the Anthropocene where the human species is the driving bio-geo-chemical force for ecological change; (Crutzen, 2006; Lewis & Maslin, 2015). So great is human influence on the planet that some scientists describe our influence on the natural order of the planet as the ‘great acceleration’ (Steffen et al., 2007), whereby at least five planetary system boundaries including climate change, biosphere integrity measured by planetary genetic diversity under what is currently the world’s sixth largest mass extinction, land-system change (i.e. altering natural systems and land cover into other forms that may be incommensurable with the provisioning and regulating services of any given ecosystem), and disruption to biogeochemical flows of nitrogen and phosphorus which regulate numerous processes required to support life on the planet (Steffen et al., 2015).
Growing attention is being paid to the pathways by which environmental or ecological change influences health through the disruption or alteration of ecosystem services (Fisher et al. 2009). Ecosystem services refer to the things that nature provides which allow life to sustain on the planet (De Groot et al., 2002). Food security and water security depend on ecosystem services. Typically, ecosystem services are grouped into several categories of services. Provisioning services refer to the production of food and water for human and non-human species, but also the production of genetic resources and energy. Regulating services regulate control ecosystems and biophysical systems so that they operate within safe limits, such as the regulation of the climate system through carbon sequestration, waste decomposition, or pest and disease control. Supporting services make it possible for services to continue to function through nutrient cycling, habitat provision or pollination, enabling ecosystems to provide other services including both provision and regulation. Cultural services refer to the spiritual, cultural, therapeutic and recreational services provided by nature, predominantly to human populations (Duraiappah et al., 2005).
It can be argued that those fortunate enough to live in countries in stages of advanced capitalism (e.g. primarily the so-called ‘Western’ or ‘Industrialized’ countries) are buffered from the ecological pressures that modify ecosystem services, through infrastructure, social and health services and emergency response management build adaptive capacity to adverse ecological change. Even so, the rate and scale of social and ecological change in a range of contexts is driving growing attention to ecosystem services as a way to understand health impacts across scales (Horwitz & Parkes, 2016) and examples of the health impacts of altering and protecting ecosystem services are expanding (McFarlane et al., in press). Despite the fact that ecosystems are non-negotiable foundations for health and well-being across the planet (Horwitz & Parkes, 2016), much of the attention to, and most pronounced health impacts of, altered ecosystem services will unfold (like the health security discourse) in lower- and middle-income countries. In these contexts, health security challenges are compounded by the fact that capacity for addressing health and its determinants may be more limited compared to The Organisation for Economic Co-operation and Development (OECD) nations, further undermining efforts directed towards the Sustainable Development Goals (see Chapter 3).
For example, Yemen’s on-going humanitarian crisis stems largely from drought conditions that have left 17 million people without adequate nutrition leading to both malnutrition and outbreaks of cholera. The humanitarian crisis in Syria, that — at the time of writing this chapter — continues to unfold, was largely driven by civil discontent stemming from the confluence of dissatisfaction with President Bashar al-Assad and the most intense period of drought Syria had ever recorded resulting in crop failures, rising food prices and migration from the countryside to the city. This ultimately led to a civil war and the need for a mass relocation of 13.5 million Syrians requiring humanitarian assistance, further highlighting the human security dimensions of prolonged environmental change (i.e. drought) which can lead to violent conflict (Barnett & Adger, 2007). Less dramatic has been the situation of Capetown in South Africa, the first city to approach ‘Day Zero’ — the day when the city would run out of potable water due to prolonged drought — triggering a series of water restrictions and the need to visit local pumps through a quota system.
Western Africa’s economy was crippled during the 2014 Ebola crisis that killed 11 000 and resulted in US$3 billion in economic losses across the region (Nkengasong et al., 2017). Ebola was driven by fragmentation of West African rain forests through expansion of resource development projects, increasing interaction among animals and humans resulting in incident cases (Rulli et al., 2017) and subsequent rapid rise in incidence (Jones et al., 2013). The spread of infectious diseases such as Ebola also requires significant multilateral containment efforts to be coordinated across the region and internationally (Davies et al., 2015; Kalra et al., 2014; WHO, 2016).
17.3.3 Potential Synergies: Linking Social-ecological Insights with Health Security
Each of the examples listed above demonstrate the complexity in linking large scale, slow moving ecological changes to processes of social change and its impacts on human health in particular global regions. However, no place on the planet is entirely devoid of the health risks from ecological change, but many of the impacts to health security will be place-specific whereby ecological change will interact with unique social and ecological contexts, along with inequities between and within population groups according to the determinants of health and interactions therein (MacIntyre et al., 2018). In other words, the social and ecological components of SES will influence place-specific vulnerabilities and adaptive capacity which ultimately influence the resilience of that system to promote good outcomes for people, other species and the environment (Ellis et al., 2018; Stokols, 1996). Examples of these variations includes the range of responses across Australia, Canada, Europe and the United States, to the expanding impact of significant forest fires in the last decade in association with changing climate (Abatzoglou et al., 2018; Tett et al., 2018). These fires result in loss of life, property and livelihoods with significant implications for mental health and accessing health services during emergencies (Dodd et al., 2018). Climate change further drives extreme heat events, violent weather, and floods and storm surges that are increasingly affecting coastal communities, which each bear impacts that are disproportionately felt by those already most disadvantaged in our society (Watts et al., 2017; Watts et al., 2018).
Thus, the coupled social and ecological change will precipitate further concern for the health of individuals and populations, including a range of equity concerns (consider social and environmental equity, intergenerational equity and interspecies equity), which will, in turn, challenge governance responses to build adaptive capacity among the most vulnerable (Quinn & Kumar, 2014). Not only will these health issues be differentially distributed across population groups and non-human species (environmental and ecological injustice (Low & Gleeson, 1998)), but they will accompany job insecurity and significant psychosocial risks which constitute additional health security threats through direct morbidity and mortality within and between population groups, resulting in rising health and social system costs as we struggle to adapt and respond to ecological change.
These examples underscore a key insight for health security that can be gleaned from understanding of contextual challenges and implications of SES: that is a need for more nuanced attention to the challenge of health security concerns across different scales (see Buse, Smith, et al., 2018), and — in particular — the need to consider social-ecological change and health security concerns, not only at the planetary, or the most local, but also at mesoscale (Galway et al., 2016; Horwitz & Parkes, 2019.
17.4 Case Examples Linking Social-ecological Insights with Human Security in Particular Bioregions
Building on the examples above, we now turn to two specific examples at the meso-scale to grapple with the complexity of health security in particular social-ecological contexts. The meso-scale here refers to intermediate scales that tend to include unique micro-climates, watersheds or specific ecological biomes, but which may cross multiple human jurisdictions including local governance. Here, we utilize meso-level examples due to their inherent linkages between both the social and the ecological in manifesting health security risks.
17.4.1 Food Security in East Africa
Food security and human security are intimately related, with both having direct implications for health security (FAO, 2016). Some human security specialists have argued for “redefining food security in terms of securing vulnerable populations from the structural violence of hunger” (Shepherd, 2012, p. 28). Global food riots are a particularly strong exemplar of coupled social-ecological systems. As Berazneva and Lee state:
a sharp escalation in worldwide commodity prices precipitated the global food crisis of 2007–2008, affecting the majority of the world’s poor, causing protests in developing countries and presenting policymakers with the challenge of simultaneously addressing hunger, poverty, and political instability. (2013, p. 28)
Examining the inter-country variability in Africa, where a majority of the population are episodically food insecure, and about one quarter are chronically food insecure, they found that “higher levels of poverty (as proxied by the [country’s] Human Poverty Index), restricted access to and availability of food, urbanization, a coastal location, more oppressive regimes and stronger civil societies were associated with a higher likelihood of riots occurring” (p. 28).
Yet ongoing climate variability (environmental insecurity) and conflict (socio-political insecurity) also have effects on food prices, and hence food security. Raleigh and colleagues (2015) honed in on markets of the main trading town of first level administration districts in 24 African states with reported political violence January 1997 to April 2010. They found that “feedback exists between food price and political violence: higher food prices increase conflict within markets, and conflict increases food price. Lower than expected levels of rainfall directly increase food price and indirectly increase conflict through its impact on food price” (p. 188).
The Integrated Food Security Phase Classification (IPC) integrates complex analyses of food insecurity and malnutrition situations. A related organization, FEWS NET, hosts a Famine Early Warning System (FEWS) network map of East Africa. An interactive world map of food security can also be accessed that shows regional food insecurity classifications in acute and chronic contexts.
These quantitative empirical findings are reflected in maps of ongoing acute food insecurity produced by the Famine Early Warning System Network (FEWS, 2019). Focusing in on East Africa, the update shows areas of both intense conflict and emergency levels of acute food insecurity (i.e. South Sudan), along with areas of ongoing crisis (e.g., Somalia), and those that are stressed (e.g. Kenya).
Particularly in such contexts, United Nations organizations have agreed to human security approaches to food security (FAO, 2016). In a narrative review on conflict and climate change, Brown and Crawford (2009) note that “reductions in crop yields and increasingly unpredictable weather patterns around the world may lead to higher prices for food and greater food insecurity” labelling climate “a ‘threat multiplier’ that makes existing concerns, such as water scarcity and food insecurity, more complex and intractable” (p. 2).
Huish (2008) has argued that “In the process of building common language between researchers and policy‐makers, the agreed definition of food security [has] excluded many important issues. As a result, the excluded, more radical issues have been pursued by off‐shoot movements that do less to directly engage the policy‐making process with existing policy‐making technocracy” (p. 1386). An example would be combined multinational corporation – government aid approaches which focus primarily on technology and markets, often not reaching the more vulnerable, African smallholder agricultural producers nor responding to their concerns (Rajaonarison, 2014).
The requirements for food security and environmental sustainability over the longer term have been set out globally (Cole et al., 2013). They include access to land, water, appropriate agricultural inputs, fair markets and supportive governance. Specific challenges and opportunities have been explored in East Africa in both urban (Yeudall et al., 2007 and more rural contexts (Braitstein et al., 2017), where the role of access to land, diverse agricultural production, promotion of dietary diversity, and human rights, including the right to food, have been given stronger emphasis. The latter are more consonant with some of the more radical approaches which Huish mentions, such as food sovereignty (Torrez, 2011) which explicitly frame the achievement of food security in social movement terms.
17.4.2 Cumulative Impacts of Multiple Resource Development Operations in Northern British Columbia
As indicated above, global land system change is significant, and largely occurring as a result of industrial agriculture and large-scale resource development projects. Resource development impacts human health through a variety of biophysical, but also social, ecological, cultural and economic pathways (Aalhus, 2017). This is a challenging conundrum for communities which are predominantly rural and remote, and rely almost exclusively on resource development pathways for local economic development (Bowles & Wilson, 2015; Halseth, 2015; Halseth & Markey, 2009).
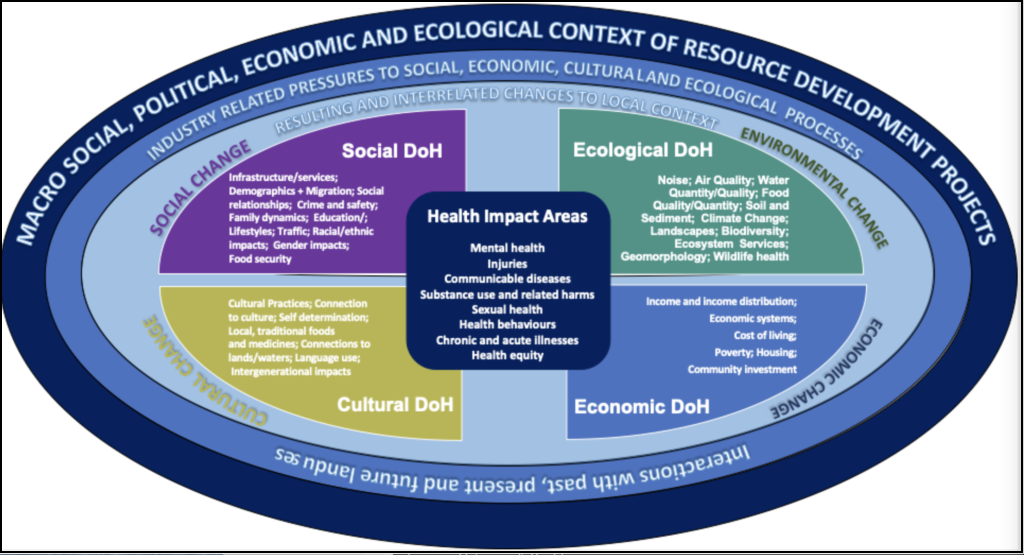
Figure 17.1 demonstrates how changing environmental conditions can produce reciprocal and interrelated changes across local contexts. These impacts to the determinants of health (DoH) thereby modify existing relationships between people and the land in ways that may create differential exposure to harm (i.e. living within close proximity to newly developed sour gas wells, or relying on an aquifer that risks contamination from multiple natural gas fracking operations) or modify risk factors in a local context (Buse et al., 2019). For example, the boom and bust dynamics of resource development can create large influxes of workers to a community without necessarily increasing services (Mactaggart et al., 2016; Shandro et al., 2011). This can lead to service-based stress, rising rates of substance use, homelessness and risks for women and children. During a bust, health services that were already functioning with limited capacity may see cuts that limits the ability of a community to address the social impacts left behind by resource development booms (Amnesty International, 2016; Buse et al., 2019).
These issues become relevant to health security when and where local systems are unable to protect and promote human health. This is particularly salient in regions with multiple forms of resource development operating on the same land base which may produce cumulative environmental, community and health impacts (Gillingham et al., 2016). Cumulative impacts have been referred to as “death by a thousand cuts” or the “tyranny of small decisions” (Noble, 2010), and conceptualize how past, present and future development projects can interact with pre-existing land-uses in ways that create both positive and negative impacts for people, their health and the broader environments in which they are situated.
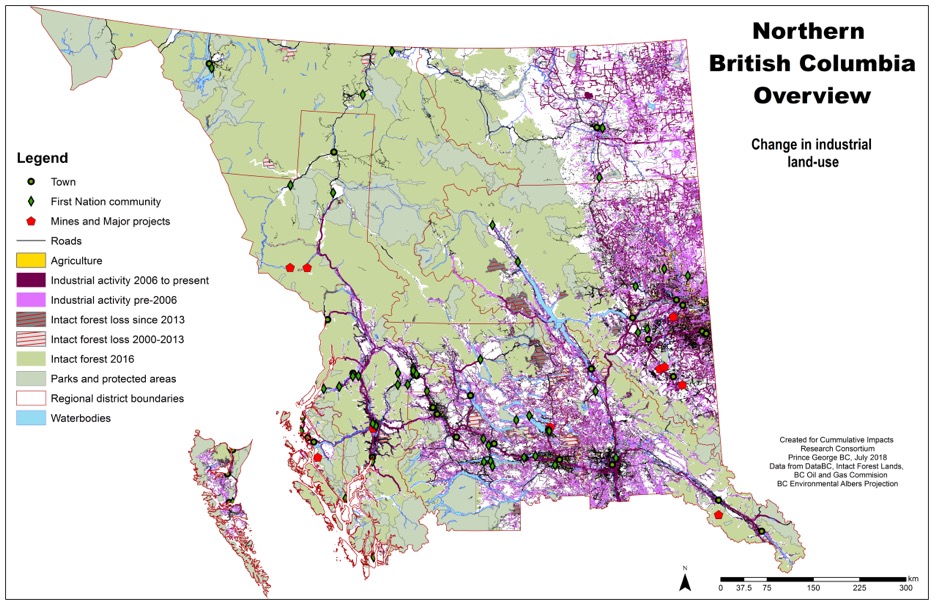
For example, Figure 17.2 illustrates an array of natural resource projects and supporting infrastructure developed across Northern British Columbia, Canada. Not only do each of the individual projects — whether a mine, hydroelectric facility, natural gas well or pipeline, and associated right of ways in the form of roads, railways and power lines — produce individual risks to human health, it is the confluence of multiple projects that poses new and emergent risks for health and the overall economic, political, social and health security of a population at a regional level, but particularly those regions that have a high dependency on natural resource operations as a principal economic driver, and where the land provides opportunities to exploit multiple types of natural resources.
Consider a simple example: the air quality and resulting respiratory health impacts of living adjacent to natural gas wells may put an individual at a certain degree of risk, living in a community that already had a smelter, pulp and paper mill, or a history of poor air quality can create new cumulative exposures for individuals and populations alike. However, these physical impacts can also be unpacked and understood in relation to other forms of cumulative impacts that have accumulated over decades and sometimes even centuries. For example, colonial impacts to Indigenous communities across the world are well-understood, and manifest in a variety of health impacts stemming from violence, trauma and a loss of culture (Greenwood et al., 2015). When combined with new environmental exposures from the earlier air quality example, a double injustice occurs, whereby determinants of health come into direct interaction with biophysical exposures producing new types of health impacts, challenges for health services delivery, or for the ability to access and benefit from ecosystem services that are inhibited by industrial change processes.
The two meso-scale case-examples presented here, offer multiple entry-points from which to explore both health security and SES. Related meso-scale case-examples have been found to be useful in a range of teaching and learning contexts that both directly and indirectly address issues relevant the interface of health security and SES, as exemplified the decade of work in the Canadian Community of Practice in Ecosystem Approaches to Health (CoPEH-Canada) (see Cole et al., 2018; Parkes et al., 2017). Since 2016, CoPEH-Canada has run a multi-institutional hybrid course (Cole et al., 2018), and has consistently used the meso-scale of watersheds as a social-ecological systems context from which to explore course themes, connecting across institutional contexts in relation to themes of “The role of universities in progressing health within their watersheds” in 2016-2018 and “Health of humans and other species in their watersheds” in 2019. Both conceptual and field-based examples and experiences can be used to explore and appreciate the SES features of these meso-scales, and also to ‘zoom-in’ and ‘zoom-out’ to consider the benefits of examining related issues at multiple scales, including the use of ‘extension activities’ and exercises such as those presented below (see also Buse, Smith, et al., 2018; Galway et al., 2016; Parkes & Horwitz, 2016).
17.5 Discussion
Environmental changes can modify health and its determinants in ways that produce security and governance challenges from the local to the global scale. From the standpoint of human security, this chapter has exemplified that security risks related to health have primarily been conceptualized in relation to emergent biological threats, but that a conceptualization of social-ecological systems encourages us to consider dimensions of time and space in manifesting systems vulnerabilities and its ability to adapt to change.
Environmental change will exacerbate existing inequities, and will also produce emergent implications for human health and the public and acute care response system to identify threats that may not be immediate, but long term and unfolding over broad geographic areas rather than resulting from a single point of origin. The time and space considerations here are significant, given that environmental change will continue to unfold in perpetuity, affecting different bioregions of the planet and the populations that reside there in nuanced and highly contextual ways. Moreover, it raises significant questions about how to promote environmental health in ways that are just and fair, thereby requiring an ethical analysis of the equity impacts of change across different scales (i.e. local, regional, national, international, planetary), but also the governance responses to promoting sustainability and mitigating or adapting to associated health impacts (Buse, Smith, et al., 2018). If normative dimensions of the health security discourse remain focused on the emergence and treatment of direct, biophysical risks to human populations, we risk limiting our response to much larger, slower-moving emergencies that will undoubtedly affect all life on the planet.
17.5.1 Towards Integrative Approaches to Health Security and Social-ecological Change
Fortunately, scholarship linking environmental and ecological contexts to the health of human and non-human entities has grown considerably over the past 150 years (Buse, Oestreicher, et al., 2018). For example, Buse, Oestreicher, et al. (2018) outline the emergence of seven ‘fields’ of environmental public health practice that simultaneously seek to address the disease/host interface present across much of the health security discourse, but to consider those interactions across nested ecological scales in ways that are attentive to equity and justice (see Figure 17.3). These fields are further built upon by Oestreicher et al. (2018) to conceptualize a variety of scholarly and applied disciplines actively working to understand and respond to the health risks posed by environmental change.
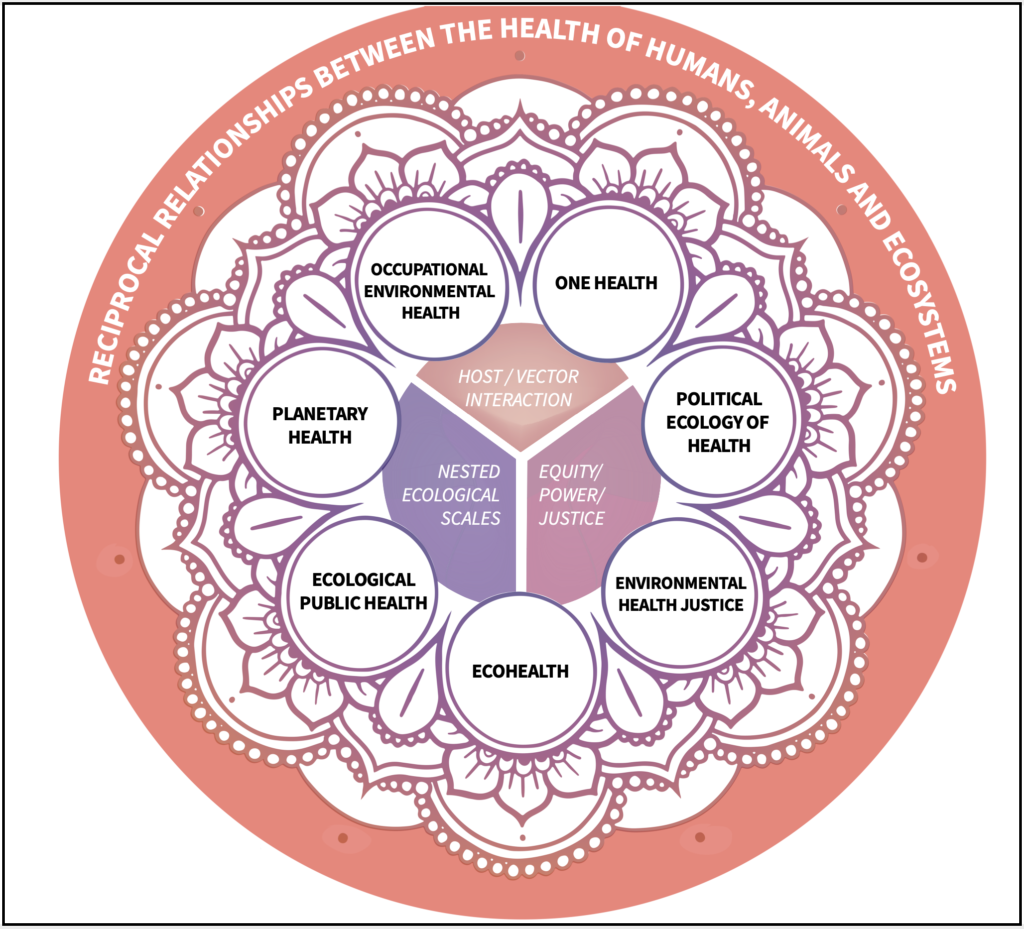
Human and health security has not necessarily been at the fore of any one of these field developments, but is implicit to their study. In the above section on health security, we see that it is often framed in response to an emerging threat (e.g. climate refugees and mass migrations, exposure to pandemic influenza) that rely on the interaction between a broader physical context and the human body. However, understanding how fields and systems are nested within one another encourages the consideration of the determinants of health, and how health promoting and protecting resources may unfairly benefit some segments of society relative to others. In other words, each of these fields, by virtue of their engagement with health and its determinants, implicitly understands that the health and security of a population is a fundamental and orienting goal of many public health responses to various crises.
17.5.2 Recommendations for Future Research, Education and Practice
What is clear from the analysis above is the emergence of several trajectories and priorities for research and capacity-strengthening to support policies and practices that can promote health security in a time of profound environmental change. First, there is an analytic requirement for health security to more fulsomely engage with existing definitions of health security in ways that account for its social, political, economic and environmental determinants. Conventional definitions overly privilege direct, biophysical risks to human health, perhaps risking considerations of the emergent, distal, and indirect risks to health and well-being posed by unique interactions among specific places and determinants of health. Broadening the health security definition is particularly helpful in recognizing environmental change as a considerable threat to health security in the 21st century. Not only will humanity continue to struggle to adapt to the impacts of climate change and a host of other bio-geo-chemical change processes that threaten our very existence if left unaddressed, but such a definition would necessarily broaden the spatial and temporal purview of health security. Indeed, many of the ecological threats to human health discussed in this chapter are playing out on timescales that not only create direct and immediate health risks, but they will continue to do so, changing and evolving in form and severity, over the course of generations. Recognizing slow moving emergencies as inherent risks to health security that unfold over diverse parts of the planet is essential given the spatial and equity dynamics at play.
Second, concerted research attention needs to be directed towards the equity dimensions of health security responses to the health impacts of environmental change, but also conventional biosecurity threats such as weapons of mass destruction and biological agents. Many of the health security threats unfolding around the world disproportionately affect low and middle-income countries due to significant capacity and infrastructure challenges, despite much of the world’s pollution and ecological threshold exceedances being driven by high-income countries’ past rapid industrial growth, and middle-income countries’ current growth. The health equity impacts of environmental change are well-studied, but further policy guidance on promoting equitable responses to health security issues, including weighing multiple trade-offs across multiple emergencies operating at different regional and temporal scales, is desperately needed. Research that seeks to unpack the equity dimensions of a just and equitable response to the health security implications of global environmental change must ask important questions about the distribution of resources and populations serviced by interventions. This is of particular relevance in contexts defined by colonial histories of physical and cultural violence, particularly against Indigenous populations, or where pre-existing population groups are differentially exposed to an environmental harm through unjust land-use or zoning policies. Ensuring a fair and equitable process is therefore central to the pursuit of environmental health justice, and is a rich area for future research on health security.
Third, there is considerable need for capacity-strengthening efforts that promote integrative understandings of health, human security and the drivers and impacts of environmental change. The discussion throughout this chapter has demonstrated the myriad ways in which health outcomes manifest from ecological change processes, but also the ways in which they produce security threats for individuals, regions, nation states and the broader international community. In embracing a definition of health security that includes the determinants of health, we draw attention to the integrative imperatives that cross-cut spatial, temporal, sectoral, value-based and disciplinary responses to security threats (see Table 17.1).
| INTEGRATED ELEMENTS | DIMENSION | EXAMPLES |
|---|---|---|
| Multiple scales | Spatial | Local, regional, national, international, planetary |
| Multiple points in time | Temporal | Past, present, future |
| Multiple sectors | Sectoral | Industry, healthcare, public health, social services, environment, housing, social and economic development, military and national defence |
| Multiple land-use values | Value-based | Environment, community, health, culture |
| Multiple methods/approaches | Disciplinary | Qualitative, quantitative, biomedical, veterinary, social determinants, public health, political science |
17.6 Conclusion
This chapter has explored the interface of health security, social-ecological systems and environmental change in order to draw connections for the human security implications of changes to social-ecological systems and the resulting impacts on human health. We have aimed to provide an overview of a topic that is worthy of numerous volumes of text, seeking to draw attention to a range of key features to the extent this is possible in a single book chapter. A key challenge for health security, particularly in an era of growing natural and anthropogenic environmental change, is to promote effective action across sectors and disciplines to promote intersectoral action in ways that support just and healthy outcomes for all; being mindful of interactions between an existing security concern and those that have existed historically but may also manifest into the future; incorporating multiple ecological, community and cultural determinants of health into an analysis of security by engaging with diverse land-use values; and leveraging lessons from multiple fields of research and practice in order to engender a nuanced understanding of health security that promotes human rights, equity and sustainability.
Resources and References
Review
Key Points
- Health security is typically conceived of as the activities required to mitigate risks, or to respond to acute events that endanger population-level health across international boundaries.
- Social-ecological systems are inextricably linked to health security, whereby both natural and anthropogenic environmental changes have cascading impacts on an array of health security issues, with some unresolvable uncertainty as to their timing, scale and distribution.
- A key challenge for health security is to promote effective action across sectors and disciplines to promote intersectoral action on the multiple environmental and community determinants of health in ways that support just and healthy outcomes for all species and humans (i.e. respecting ecological as well as environmental rights).
- Integrative approaches to understanding ecology and society and their implications for health resonate with the early conceptualizations of health security.
- Global environmental change will exacerbate existing inequities across dimensions of human security, but particularly in health status.
- A key challenge for health security, particularly in an era of growing natural and anthropogenic environmental change, is to promote effective action across sectors and disciplines to promote intersectoral action in ways that support just and healthy outcomes for all; being mindful of interactions between an existing security concern and those that have existed historically but may also manifest into the future; incorporating multiple environmental, community and cultural determinants of health into an analysis of security by engaging with diverse land-use values; and leveraging lessons from multiple fields of research to engender nuanced understandings of health security to promote human rights.
Extension Activities & Further Research
- How is climate change related to health security? Describe some examples.
- Pick a bioregion (e.g. in the lower Great Lakes or the Salish Sea in the Pacific Northwest) and describe what elements of its composite ecosystems and social systems contribute to health security or health insecurity?
- In what ways might governments work to redress the health security implications of global ecological change?
- What do you think the most important ecological and social determinants of your health are at this point in your life?
- Who is most impacted by global environmental change as it relates to health security issues?
- Scales are important and can be illustrated by a “zoom in, zoom out” mental exercise (adapted from Parkes & Horwitz, 2016):
- Think of your current environment and try to imagine both the living (biotic) and non-living (abiotic) parts interacting with another living thing, such as yourself? How do social dynamics influence these interrelationships?
- Zoom out from that specific interaction to your neighbourhood. Do you see more life yet? What other species do you see that make up this social-ecological community? What species do you not see? What things move and interact the most? How might they affect your health security?
- Zoom out farther, to the borders of the bioregion in which you are currently located. Does what you are seeing look more or less alive? Do you visualize this view as a roadmap or as a satellite image? Can you see evidence of social-ecological crises from this vantage point?
- Once you have a large-scale (regional in a continent) view in your mind’s eye, consider three questions:
- How would this view have looked different five years ago? And potentially look 10 years from now?
- Identify two positive and three negative determinants of health security for each of these time frames at this scale.
- Give three examples of where you can see (imagine?) the atmosphere (air), geosphere (rock, land) and hydrosphere (water) interacting to support life within the view you see.
- Websites that can help you experience these features of zooming in and out through social and ecological contexts include what is your ecological footprint? and The Scale of the Universe. Specific papers also explore the ways in which these dynamics may assist interdisciplinary learning (e.g. Galway et al., 2016).
List of Terms
See Glossary for full list of terms and definitions.
- bioregion
- biosecurity
- ecosystem services
- food security
- health security
- livelihoods
- meso-scale
- social-ecological systems
- water security
Suggested Reading
Charron, D. F. (Ed.). (2012). Ecohealth research in practice: Innovative applications of an ecosystem approach to health (p. 282). Springer; International Development Research Centre.
Millennium Ecosystem Assessment. (2005). Ecosystems and human well-being: Synthesis. World Resources Institute. https://www.millenniumassessment.org/documents/document.356.aspx.pdf
The Rockefeller Foundation–Lancet Commission. (2015). The Rockefeller Foundation–Lancet Commission paper on planetary health. http://www.thelancet.com/infographics/planetary-health
Rushton, S., & Youde, J. (Eds.). (2015). Routledge handbook of global health security. Routledge.
World Health Organization. (2007). The world health report 2007 – A safer future: Global public health security in the 21st century. https://www.who.int/whr/2007/en/
References
Aalhus, M., Oke, B., & Fumerton, R. (2018). The social determinants of health impacts of resource extraction and development in rural and northern communities: A summary of impacts and promising practices for assessment and monitoring. Northern Health. https://www.northernhealth.ca/sites/northern_health/files/services/office-health-resource-development/documents/impacts-promising-practices-assessment-monitoring.pdf
Abatzoglou, J. T., Williams, A. P., & Barbero, R. (2018). Global emergence of anthropogenic climate change in fire weather indices. Geophysical Research Letters, 46(1), 326–336. https://doi.org/10.1029/2018GL080959
Aldis, W. (2008). Health security as a public health concept: A critical analysis. Health Policy and Planning, 23(6), 369–375. https://doi.org/10.1093/heapol/czn030
Amnesty International. (2016). Out of sight, out of mind: Gender, Indigenous rights, and energy development in northeast British Columbia, Canada (AMR 20/4872/2016). https://www.amnesty.org/en/documents/amr20/4872/2016/en/
Andrachuk, M., & Armitage, D. (2015). Understanding social-ecological change and transformation through community perceptions of system identity. Ecology and Society, 20(4), Article 26. https://doi.org/10.5751/ES-07759-200426
Balajee, S. A., Arthur, R., & Mounts, A. W. (2016). Global health security: Building capacities for early event detection, epidemiologic workforce, and laboratory response. Health Security, 14(6), 424–432. https://doi.org/10.1089/hs.2015.0062
Bambery, Z., Cassell, C. H., Bunnell, R. E., Roy, K., Ahmed, Z., Payne, R. L., & Meltzer, M. I. (2018). Impact of a hypothetical infectious disease outbreak on US exports and export-based jobs. Health Security, 16(1), 1–7. https://doi.org/10.1089/hs.2017.0052
Barnett, J., & Adger, W. N. (2007). Climate change, human security and violent conflict. Political Geography, 26(6), 639–655. https://doi.org/10.1016/j.polgeo.2007.03.003
Belay, E. D., Kile, J. C., Hall, A. J., Barton-Behravesh, C., Parsons, M. B., Salyer, S. J., & Walke, H. (2017). Zoonotic disease programs for enhancing global health security. Emerging Infectious Diseases, 23(13). https://doi.org/10.3201/eid2313.170544
Berazneva, J., & Lee, D. R. (2013). Explaining the African food riots of 2007–2008: An empirical analysis. Food Policy, 39(C), 28–39. https://doi.org/10.1016/j.foodpol.2012.12.007
Berbés-Blázquez, M., Oestreicher, J. S., Mertens, F., & Saint-Charles, J. (2014). Ecohealth and resilience thinking: A dialog from experiences in research and practice. Ecology and Society, 19(2), Article 24. https://doi.org/10.5751/ES-06264-190224
Berkes, F., Colding, J., & Folke, C. (Eds.). (2003). Navigating social-ecological systems: Building resilience for complexity and change. Cambridge University Press. https://doi.org/10.1017/CBO9780511541957
Bond, K. (2008). Health security or health diplomacy? Moving beyond semantic analysis to strengthen health systems and global cooperation. Health Policy and Planning, 23(6), 376–378. https://doi.org/10.1093/heapol/czn031
Borchert, J. N., Tappero, J. W., Downing, R., Shoemaker, T., Behumbiize, P., Aceng, J., Makumbi, I., Dahlke, M., Jarrar, B., Lozano, B., Kasozi, S., Austin, M., Phillippe, D., Watson, I. D., Evans, T. J., Stotish, T., Dowell, S. F., Iademarco, M. F., Ransom, R., … Wuhib, T. (2014). Rapidly building global health security capacity: Uganda Demonstration Project, 2013. Morbidity and Mortality Weekly Report, 63(4), 73–76. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6304a2.htm
Bowles, P., & Wilson, G. N. (Eds.). (2015). Resource communities in a globalizing region: Development, agency, and contestation in northern British Columbia. UBC Press.
Braitstein, P., Lama, T., Keino, S., Gladanac, B., Yego, F., Cole, D., Tabu, J. S., Cortinois, A., Tarus, C., & Fox, A. (2017). Increasing food security and nutrition resilience in response to climate change in east Africa: Findings from a multisectoral symposium. The Lancet Global Health, 5(S23). https://doi.org/10.1016/S2214-109X(17)30130-4
Brown, O., & Crawford, A. (2009). Climate change and security in Africa: A study for the Nordic-African foreign ministers meeting. International Institute for Sustainable Development. https://www.iisd.org/publications/climate-change-and-security-africa
Bunch, M. J., Morrison, K. E., Parkes, M. W., & Venema, H. D. (2011). Promoting health and well-being by managing for social–ecological resilience: The potential for integrating ecohealth and water resources management approaches. Ecology and Society, 16(1), Article 6. http://www.ecologyandsociety.org/vol16/iss1/art6/
Buse, C. G., Oestreicher, J. S., Ellis, N. R., Patrick, R., Brisbois, B., Jenkins, A. P., McKellar, K., Kingsley, J., Gislason, M., Galway, L., McFarlane, R. A., Walker, J., Frumkin, H., & Parkes, M. (2018). Public health guide to field developments linking ecosystems, environments and health in the Anthropocene. Journal of Epidemiology and Community Health, 72(5), 420–425. https://doi.org/10.1136/jech-2017-210082
Buse, C. G., Sax, M., Nowak, N., Jackson, J., Fresco, T., Fyfe, T., & Halseth, G. (2019). Locating community impacts of unconventional natural gas across the supply chain: A scoping review. The Extractive Industries and Society, 6(2), 620–629. https://doi.org/10.1016/j.exis.2019.03.002
Buse, C. G., Smith, M., & Silva, D. S. (2018). Attending to scalar ethical issues in emerging approaches to environmental health research and practice. Monash Bioethics Review, 37(1–2), 4–21. https://doi.org/10.1007/s40592-018-0080-3
Cameron, E. E. (2017). Emerging and converging global catastrophic biological risks. Health Security, 15(4), 337–338. https://doi.org/10.1089/hs.2017.0043
Carr, E. R. (2015). Political ecology and livelihoods. In T. Perreault, G. Bridge, & J. McCarthy (Eds.), The Routledge handbook of political ecology handbook (pp. 332–342). Routledge.
Carus, W. S. (2015). The history of biological weapons use: What we know and what we don’t. Health Security, 13(4), 219–255. https://doi.org/10.1089/hs.2014.0092
Chambers, R., & Conway, G. R. (1992). Sustainable rural livelihoods: Practical concepts for the 21st century (IDS Discussion Paper 296). Institute of Development Studies. https://www.ids.ac.uk/publications/sustainable-rural-livelihoods-practical-concepts-for-the-21st-century/
Chan, M. (2009). Primary health care as a route to health security. The Lancet, 373(9675), 1586–1587. https://doi.org/10.1016/S0140-6736(09)60003-9
Chandra, A., Acosta, J. D., Meredith, L. S., Sanches, K., Howard, S., Uscher-Pines, L., Williams, M. V., & Yeung, D. (2010). Understanding community resilience in the context of national health security: A literature review (WR-737-DHHS). RAND Corporation. https://www.rand.org/pubs/working_papers/WR737.html
Chen, L., & Narasimhan, V. (2003). Human security and global health. Journal of Human Development, 4(2), 181–190. https://doi.org/10.1080/1464988032000087532
Cole, D. C., Eyles, J., Gibson, B. L., & Ross, N. (1999). Links between humans and ecosystems: The implications of framing for health promotion strategies. Health Promotion International, 14(1), 65–72. https://doi.org/10.1093/heapro/14.1.65
Cole, D. C., Parkes, M. W., Saint-Charles, J., Gislason, M., McKellar, K., & Webb, J. (2018). Evolution of capacity strengthening: Insights from the Canadian community of practice in ecosystem approaches to health. Transformative Dialogues: Teaching & Learning Journal, 11(2), 1–21. https://www.kpu.ca/sites/default/files/Transformative%20Dialogues/TD.11.2_Cole_etal_Evolution_of_capacity_strengthening.pdf
Cole, D. C., Prain, G., & Pradel, W. (2013). Healthy and sustainable agriculture: Working with farmers to transform food production in Latin America. In J. Heymann & M. Barrera (Eds.), Ensuring a sustainable future: Making progress on environment and equity (pp. 189–220). Oxford University Press.
Colf, L. A. (2016). Preparing for nontraditional biothreats. Health Security, 14(1), 7–12. https://doi.org/10.1089/hs.2015.0045
Commission on Social Determinants of Health. (2008). Closing the gap in a generation: Health equity through action on the social determinants of health. World Health Organization. https://www.who.int/social_determinants/thecommission/finalreport/en/
Cote, M., & Nightingale, A. J. (2012). Resilience thinking meets social theory: Situating social change in socio-ecological systems (SES) research. Progress in Human Geography, 36(4), 475–489. https://doi.org/10.1177/0309132511425708
Cretney, R. (2014). Resilience for whom? Emerging critical geographies of socio-ecological resilience. Geography Compass, 8(9), 627–640. https://doi.org/10.1111/gec3.12154
Crutzen, P. J. (2006). The “Anthropocene”. In E. Ehlers & T. Krafft (Eds.), Earth system science in the Anthropocene: Emerging issues and problems (pp. 13–18). Springer.
Davies, S. E., Kamradt-Scott, A., & Rushton, S. (2015). Disease diplomacy: International norms and global health security. Johns Hopkins University Press.
de Groot, R. S., Wilson, M. A., & Boumans, R. M. J. (2002). A typology for the classification, description and valuation of ecosystem functions, goods and services. Ecological Economics, 41(3), 393–408. https://doi.org/10.1016/S0921-8009(02)00089-7
Dodd, W., Scott, P., Howard, C., Scott, C., Rose, C., Cunsolo, A., & Orbinski, J. (2018). Lived experience of a record wildfire season in the Northwest Territories, Canada. Canadian Journal of Public Health, 109(3), 327–337. https://doi.org/10.17269/s41997-018-0070-5
Edwards, N., & Davison, C. (2015). Strengthening communities with a socio-ecological approach: Local and international lessons in whole systems. In L. K. Hallström, N. P. Guehlstorf, & M. W. Parkes (Eds.), Ecosystems, society, and health: Pathways through diversity, convergence, and integration (pp. 33–67). McGill–Queen’s University Press.
Eisenmann, D. P., Wold, C., Setodji, C., Hickey, S., Lee, B., Stein, B. D., & Long, A. (2004). Will public health’s response to terrorism be fair? Racial/ethnic variations in perceived fairness during a bioterrorist event. Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science, 2(3), 146–156. https://doi.org/10.1089/bsp.2004.2.146
Ellis, E. C., Magliocca, N. R., Stevens, C. J., & Fuller, D. Q. (2018). Evolving the Anthropocene: Linking multi-level selection with long-term social–ecological change. Sustainability Science, 13(1), 119–128. https://doi.org/10.1007/s11625-017-0513-6
Errett, N. A., Egan, S., Garrity, S., Rutkow, L., Walsh, L., Thompson, C. B., Strauss-Riggs, K., Altman, B., Schor, K., & Barnett, D. J. (2015). Attitudinal determinants of local public health workers’ participation in Hurricane Sandy recovery activities. Health Security, 13(4), 267–273. https://doi.org/10.1089/hs.2015.0004
Famine Early Warning System Network. (2019). East Africa food security outlook: Conflict and production deficits to drive deterioration in food security through at least May. http://fews.net/east-africa/food-security-outlook-update/march-2019
Feldbaum, H., & Lee, K. (2004). Public health and security. In A. Ingram (Ed.), Health, foreign policy and security: Towards a conceptual framework for research and policy (pp. 19–28). The Nuffield Trust. https://www.nuffieldtrust.org.uk/files/2017-01/health-foreign-policy-and-security-web-final.pdf
Fidler, D. P. (2007). A pathology of public health securitism: Approaching pandemics as security threats. In A. F. Cooper, J. J. Kirton, & T. Schrecker (Eds.), Governing global health: Challenge, response, innovation (pp. 41–66). Routledge.
Fisher, B., Turner, R. K., & Morling, P. (2009). Defining and classifying ecosystem services for decision making. Ecological Economics, 68(3), 643–653. https://doi.org/10.1016/j.ecolecon.2008.09.014
Fitzmaurice, A. G., Mahar, M., Moriarty, L. F., Bartee, M., Hirai, M., Li, W., Russell Gerber, A., Tappero, J. W., Bunnell, R., & GHSA Implementation Group. (2017). Contributions of the US Centers for Disease Control and Prevention in implementing the global health security agenda in 17 partner countries. Emerging Infectious Diseases, 23(13). https://doi.org/10.3201/eid2313.17089
Folke, C. (2006). Resilience: The emergence of a perspective for social–ecological systems analyses. Global Environmental Change, 16(3), 253–267. https://doi.org/10.1016/j.gloenvcha.2006.04.002
Food and Agriculture Organization. (2016). Human security & food security (No. I5522E/1/03.16). www.fao.org/3/a-i5522e.pdf
Frieden, T. R., Tappero, J. W., Dowell, S. F., Hien, N. T., Guillaume, F. D., & Aceng, J. R. (2014). Safer countries through global health security. The Lancet, 383(9919), 764–766. https://doi.org/10.1016/S0140-6736(14)60189-6
Galway, L. P., Parkes, M. W., Allen, D., & Takaro, T. K. (2016). Building interdisciplinary research capacity: A key challenge for ecological approaches in public health. AIMS Public Health, 3(2), 389–406. https://doi.org/10.3934/publichealth.2016.2.389
Gillingham, M. P., Halseth, G. R., Johnson, C. J., & Parkes, M. W. (Eds.). (2016). The integration imperative: Cumulative environmental, community and health effects of multiple natural resource developments. Springer. https://doi.org/10.1007/978-3-319-22123-6
Gostin, L. O., & Katz, R. (2016). The international health regulations: The governing framework for global health security. The Milbank Quarterly, 94(2), 264–313. https://doi.org/10.1111/1468-0009.12186
Greenwood, M., de Leeuw, S., Lindsay, N. M., & Reading, C. (Eds.). (2015). Determinants of Indigenous peoples’ health in Canada: Beyond the social. Canadian Scholars’ Press.
Gunderson, L. H. (2010). Ecological and human community resilience in response to natural disasters. Ecology and Society, 15(2), Article 18. http://www.ecologyandsociety.org/vol15/iss2/art18/
Gunderson, L. H., & Holling, C. S. (Eds.). (2001). Panarchy: Understanding transformations in human and natural systems. Island Press.
Halseth, G. R. (2015). Cumulative effects and impacts: Introducing a community perspective. In M. P. Gillingham, G. R. Halseth, C. J. Johnson, & M. W. Parkes (Eds.), The integration imperative: Cumulative environmental, community and health effects of multiple natural resource developments (pp. 83–115). Springer. https://doi.org/10.1007/978-3-319-22123-6_4
Halseth, G., & Markey, S. (2009). Understanding and transforming a staples-based economy: Place-based development in northern British Columbia, Canada. In G. R. Halseth, S. Markey, & D. Bruce (Eds.), The next rural economies: Constructing rural place in global economies (pp. 251–262). CABI International.
Hoffman, S. J. (2010). The evolution, etiology and eventualities of the global health security regime. Health Policy and Planning, 25(6), 510–522. https://doi.org/10.1093/heapol/czq037
Holling, C. S. (1986). The resilience of terrestial ecosystems: Local surprise and global change. In W. C. Clark & R. E. Munn (Eds.), Sustainable development of the biosphere (pp. 292–317). International Institute for Applied Systems Analysis; Cambridge University Press. http://pure.iiasa.ac.at/id/eprint/2751/
Holling, C. S. (2001). Understanding the complexity of economic, ecological, and social systems. Ecosystems, 4(5), 390–405. https://doi.org/10.1007/s10021-001-0101-5
Horwitz, P., & Parkes, M. W. (2016). Scoping health impact assessment: Ecosystem services as a framing device. In D. Geneletti (Ed), Handbook on biodiversity and ecosystem services in impact assessment (pp. 62–85). Edward Elgar Publishing. https://doi.org/10.4337/9781783478996.00009
Horwitz, P., & Parkes, M. W. (2019). Intertwined strands for ecology in planetary health. Challenges, 10(1), Article 20. https://doi.org/10.3390/challe10010020
Huish, R. (2008). Human security and food security in geographical study: Pragmatic concepts or elusive theory? Geography Compass, 2(5), 1386–1403. https://doi.org/10.1111/j.1749-8198.2008.00155.x
Jones, B. A., Grace, D., Kock, R., Alonso, S., Rushton, J., Said, M. Y., McKeever, D., Mutua, F., Young, J., McDermott, J., & Pfeiffer, D. U. (2013). Zoonosis emergence linked to agricultural intensification and environmental change. Proceedings of the National Academy of Sciences of the United States of America, 110(21), 8399–8404. https://doi.org/10.1073/pnas.1208059110
Kalra, S., Kelkar, D., Galwankar, S. C., Papadimos, T. J., Stawicki, S. P., Arquilla, B., Hoey, B. A., Sharpe, R. P., Sabol, D., & Jahre, J. A. (2014). The emergence of Ebola as a global health security threat: From ‘lessons learned’ to coordinated multilateral containment efforts. Journal of Global Infectious Diseases, 6(4), 164–177. https://doi.org/10.4103/0974-777X.145247
Kamradt-Scott, A. (2011). The evolving WHO: Implications for global health security. Global Public Health, 6(8), 801–813. https://doi.org/10.1080/17441692.2010.513690
Kamradt-Scott, A. (2015). Managing global health security: The World Health Organization and disease outbreak control. Palgrave Macmillan. https://doi.org/10.1057/9781137520166
Katz, R., Sorrell, E. M., Kornblet, S. A., & Fischer, J. E. (2014). Global health security agenda and the international health regulations: Moving forward. Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science, 12(5), 231–238. https://doi.org/10.1089/bsp.2014.0038
Kennedy, E. D., Morgan, J., & Knight, N. W. (2018). Global health security implementation: Expanding the evidence base. Health Security, 16(S1), S-1–S-4. https://doi.org/10.1089/hs.2018.0120
Khan, A. S. (2011). Public health preparedness and response in the USA since 9/11: A national health security imperative. The Lancet, 378(9794), 953–956. https://doi.org/10.1016/S0140-6736(11)61263-4
Kull, C. A., Kueffer, C., Richardson, D. M., Vaz, A. S., Vicente, J. R., & Honrado, J. P. (2018). Using the “regime shift” concept in addressing social–ecological change. Geographical Research, 56(1), 26–41. https://doi.org/10.1111/1745-5871.12267
Kutzin, J., & Sparkes, S. P. (2016). Health systems strengthening, universal health coverage, health security and resilience. Bulletin of the World Health Organization, 94(1), 2. https://www.who.int/bulletin/volumes/94/1/15-165050/en/
Lee, K., & McInnes, C. (2004). A conceptual framework for research and policy. In A. Ingram (Ed.), Health, foreign policy and security: Towards a conceptual framework for research and policy (pp. 10–18). The Nuffield Trust. https://www.nuffieldtrust.org.uk/files/2017-01/health-foreign-policy-and-security-web-final.pdf
Levin, S. A. (1998). Ecosystems and the biosphere as complex adaptive systems. Ecosystems, 1(5), 431–436. https://doi.org/10.1007/s100219900037
Lewis, S. L., & Maslin, M. A. (2015). Defining the Anthropocene. Nature, 519(7542), 171–180. https://doi.org/10.1038/nature14258
Lo, C. Y., & Thomas, N. (2010). How is health a security issue? Politics, responses and issues. Health Policy and Planning, 25(6), 447–453. https://doi.org/10.1093/heapol/czq063
Low, N., & Gleeson, B. (1998). Justice, society and nature: An exploration of political ecology. Routledge.
MacIntyre, C. R., Engells, T. E., Scotch, M., Heslop, D. J., Gumel, A. B., Poste, G., Chen, X., Herche, W., Steinhöfel, K., Lim, S., & Broom, A. (2018). Converging and emerging threats to health security. Environment Systems and Decisions, 38(2), 198–207. https://doi.org/10.1007/s10669-017-9667-0
MacPherson, D. W., Hushulak, B. D., & Macdonald, L. (2007). Health and foreign policy: Influences of migration and population mobility. Bulletin of the World Health Organization, 85(3), 200–206. https://doi.org/10.2471/BLT.06.036962
Mactaggart, F., McDermott, L., Tynan, A., & Gericke, C. (2016). Examining health and well‐being outcomes associated with mining activity in rural communities of high‐income countries: A systematic review. The Australian Journal of Rural Health, 24(4), 230–237. https://doi.org/10.1111/ajr.12285
McFarlane, R. A., Horwitz, P., Arabena, K., Capon, A., Jenkins, A., Jupiter, S., Negin, J., Parkes, M. W., & Saketa, S. (2019). Ecosystem services for human health in Oceania. Ecosystem Services, 39, Article 100976. https://doi.org/10.1016/j.ecoser.2019.100976
McInnes, C. (2005). Health, security and the risk society. The Nuffield Trust. https://www.nuffieldtrust.org.uk/files/2017-01/health-security-and-the-risk-society-web-final.pdf
McInnes, C. (2015). The many meanings of health security. In S. Rushton & J. Youde (Eds.), Routledge handbook of global health security (pp. 7–17). Routledge.
McLaren, L., & Hawe, P. (2005). Ecological perspectives in health research. Journal of Epidemiology and Community Health, 59(1), 6–14. http://doi.org/10.1136/jech.2003.018044
Mikkonen, J., & Raphael, D. (2010). Social determinants of health: The Canadian facts. York University School of Health Policy and Management.
Millennium Ecosystem Assessment. (2005). Ecosystems and human well-being: Biodiversity synthesis. World Resources Institute. https://www.millenniumassessment.org/documents/document.354.aspx.pdf
National Aeronautics and Space Administration. (2020). Global climate change: Vital signs of the planet. Retrieved July 1, 2019, from https://climate.nasa.gov/vital-signs/global-temperature/
Nkengasong, J., Djoudalbaye, B., & Maiyegun, O. (2017). A new public health order for Africa’s health security. The Lancet Global Health, 5(11), e1064–e1065. https://doi.org/10.1016/S2214-109X(17)30363-7
Noble, B. (2010). Cumulative environmental effects and the tyranny of small decisions: Towards meaningful cumulative effects assessment and management (Natural Resources & Environmental Studies Institute Occasional Paper No. 8). University of Northern British Columbia. https://unbc.arcabc.ca/islandora/object/unbc%253A71
Novotny, T. E. (2007). Global governance and public health security in the 21st century. California Western International Law Journal, 38(1), 19–40. https://scholarlycommons.law.cwsl.edu/cwilj/vol38/iss1/6/
Oestreicher, J. S., Buse, C., Brisbois, B., Patrick, R., Jenkins, A., Kingsley, J., Távora, R., & Fatorelli, L. (2018). Where ecosystems, people and health meet: Academic traditons and emerging fields for research and practice. Sustainability in Debate, 9(1), 45–65. http://hdl.handle.net/1959.3/443669
Ostergard, R. L., Jr., & Kauneckis, D. (2014). Health security and environmental change. In S. Rushton & J. Youde (Eds.), Routledge handbook of global health security (pp. 151–162). Routledge.
Paranjape, S. M., & Franz, D. R. (2015). Implementing the global health security agenda: Lessons from global health and security programs. Health Security, 13(1), 9–19. https://doi.org/10.1089/hs.2014.0047
Parkes, M. W., & Horwitz, P. (2009). Water, ecology and health: Ecosystems as settings for promoting health and sustainability. Health Promotion International, 24(1), 94–102. https://doi.org/10.1093/heapro/dan044
Parkes, M. W., & Horwitz, P. (2016). Ecology and ecosystems as foundational for health. In H. Frumkin (Ed.), Environmental health: From global to local (3rd ed., pp. 27–58). Jossey-Bass.
Parkes, M. W., Panelli, R., & Weinstein, P. (2003). Converging paradigms for environmental health theory and practice. Environmental Health Perspectives, 111(5), 669–675. https://doi.org/10.1289/ehp.5332
Parkes, M. W., Saint-Charles, J., Cole, D. C., Gislason, M., Hicks, E., Le Bourdais, C., McKellar, K. A., Bouchard, M. S.-C., & Canadian Community of Practice in Ecosystem Approaches to Health Team. (2017). Strengthening collaborative capacity: Experiences from a short, intensive field course on ecosystems, health and society. Higher Education Research and Development, 36(5), 1031–1046. https://doi.org/10.1080/07294360.2016.1263937
Percival, V., & Homer-Dixon, T. F. (1998). Environmental scarcity and violent conflict: The case of South Africa. Journal of Peace Research, 35(3), 279–298. https://doi.org/10.1177/0022343398035003002
Quinn, S. C., & Kumar, S. (2014). Health inequalities and infectious disease epidemics: A challenge for global health security. Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science, 12(5), 263–273. https://doi.org/10.1089/bsp.2014.0032
Rajaonarison, H. M. (2014). Food and human security in sub-Saharan Africa. Procedia Environmental Sciences, 20, 377–385. https://doi.org/10.1016/j.proenv.2014.03.048
Raleigh, C., Choi, H. J., & Kniveton, D. (2015). The devil is in the details: An investigation of the relationships between conflict, food price and climate across Africa. Global Environmental Change, 32, 187–199. https://doi.org/10.1016/j.gloenvcha.2015.03.005
Rulli, M. C., Santini, M., Hayman, D. T. S., & D’Odorico, P. (2017). The nexus between forest fragmentation in Africa and Ebola virus disease outbreaks. Scientific Reports, 7, Article 41613. https://doi.org/10.1038/srep41613
Rushton, S. (2011). Global health security: Security for whom? Security from what? Political Studies, 59(4), 779–796. https://doi.org/10.1111/j.1467-9248.2011.00919.x
Schoch-Spana, M., Cicero, A., Adalja, A., Gronvall, G., Kirk Sell, T., Meyer, D., Nuzzo, J. B., Ravi, S., Shearer, M. P., Toner, E., Watson, C., Watson, M., & Inglesby, T. (2017). Global catastrophic biological risks: Toward a working definition. Health Security, 15(4), 323–328. https://doi.org/10.1089/hs.2017.0038
Shandro, J. A., Veiga, M. M., Shoveller, J., Scoble, M., & Koehoorn, M. (2011). Perspectives on community health issues and the mining boom–bust cycle. Resources Policy, 36(2), 178–186. https://doi.org/10.1016/j.resourpol.2011.01.004
Shepherd, B. (2012). Thinking critically about food security. Security Dialogue, 43(3), 195–212. https://doi.org/10.1177/0967010612443724
Sikka, V., Chattu, V. K., Popli, R. K., Galwankar, S. C., Kelkar, D., Sawicki, S. G., Stawicki, S. P., & Papadimos, T. J. (2016). The emergence of zika virus as a global health security threat: A review and a consensus statement of the INDUSEM Joint Working Group (JWG). Journal of Global Infectious Diseases, 8(1), 3–15. https://doi.org/10.4103/0974-777X.176140
Smith, A., & Stirling, A. (2010). The politics of social-ecological resilience and sustainable socio-technical transitions. Ecology and Society, 15(1), Article 11. http://www.ecologyandsociety.org/vol15/iss1/art11/
Steffen, W., Broadgate, W., Deutsch, L., Gaffney, O., & Ludwig, C. (2015). The trajectory of the Anthropocene: The Great Acceleration. The Anthropocene Review, 2(1), 81–98. https://doi.org/10.1177/2053019614564785
Steffen, W., Crutzen, P. J., & McNeill, J. R. (2007). The Anthropocene: Are humans now overwhelming the great forces of nature. AMBIO: A Journal of the Human Environment, 36(8), 614–621. https://doi.org/10.1579/0044-7447(2007)36[614:TAAHNO]2.0.CO;2
Stokols, D. (1996). Translating social ecological theory into guidelines for community health promotion. American Journal of Health Promotion, 10(4), 282–298. https://doi.org/10.4278/0890-1171-10.4.282
Tappero, J. W., Cassell, C. H., Bunnell, R., Angulo, F. J., Craig, A., Pesik, N., Dahl, B. A., Ijaz, K., Martin, R., & Global Health Security Science Group. (2017). US Centers for Disease Control and Prevention and its partners’ contributions to global health security. Emerging Infectious Diseases, 23(13). https://doi.org/10.3201/eid2313.170946
Taylor, H. A., Rutkow, L., & Barnett, D. J. (2018). Local preparedness for infectious disease outbreaks: A qualitative exploration of willingness and ability to respond. Health Security, 16(5), 311–319. https://doi.org/10.1089/hs.2018.0046
Tett, S. F. B., Falk, A., Rogers, M., Spuler, F., Turner, C., Wainwright, J., Dimdore-Miles, O., Knight, S., Freychet, N., Mineter, M. J., & Lehmann, C. E. R. (2018). Anthropogenic forcings and associated changes in fire risk in western North America and Australia during 2015/16. Bulletin of the American Meteorological Society, 99(1), S60–S64. https://doi.org/10.1175/BAMS-D-17-0096.1
Toner, E., Adalja, A., Gronvall, G. K., Cicero, A., & Inglesby, T. V. (2015). Antimicrobial resistance is a global health emergency. Health Security, 13(3), 153–155. https://doi.org/10.1089/hs.2014.0088
Torrez, F. (2011). La Via Campesina: Peasant-led agrarian reform and food sovereignty. Development, 54(1), 49–54. https://doi.org/10.1057/dev.2010.96
United Nations. (2012). Follow-up to paragraph 143 on human security of the 2005 World Summit Outcome (UN A/RES/66/290). https://www.un.org/ga/search/viewm_doc.asp?symbol=A/RES/66/290
United Nations University Institute for Water, Environment & Health. (2013). Water security & the global water agenda: A UN-Water analytical brief. https://www.unwater.org/publications/water-security-global-water-agenda/
Vietti, F., & Scribner, T. (2013). Human insecurity: Understanding international migration from a human security perspective. Journal on Migration and Human Security, 1(1), 17–31. https://doi.org/10.1177/233150241300100102
Vilhena, D. A., & Antonelli, A. (2015). A network approach for identifying and delimiting biogeographical regions. Nature Communications, 6, Article 6848. https://doi.org/10.1038/ncomms7848
Walker, B., Holling, C. S., Carpenter, S. R., & Kinzig, A. (2004). Resilience, adaptability and transformability in social–ecological systems. Ecology and Society, 9(2), Article 5. http://www.ecologyandsociety.org/vol9/iss2/art5/
Watts, N., Adger, W. N., Ayeb-Karlsson, S., Bai, Y., Byass, P., Campbell-Lendrum, D., Colbourn, T., Cox, P., Davies, M., Depledge, M., Depoux, A., Dominguez-Salas, P., Drummond, P., Ekins, P., Flahault, A., Grace, D., Graham, H., Haines, A., Hamilton, I., … Costello, A. (2017). The Lancet Countdown: Tracking progress on health and climate change. The Lancet, 389(10074), 1151–1164. https://doi.org/10.1016/S0140-6736(16)32124-9
Watts, N., Amann, M., Ayeb-Karlsson, S., Belesova, K., Bouley, T., Boykoff, M., Byass, P., Cai, W., Campbell-Lendrum, D., Chambers, J., Cox, P. M., Daly, M., Dasandi, N., Davies, M., Depledge, M., Depoux, A., Dominquez-Salas, P., Drummond, P., Ekins, P., … Costello, A. (2018). The Lancet Countdown on health and climate change: From 25 years of inaction to a global transformation for public health. The Lancet, 391(10120), 581–630. https://doi.org/10.1016/S0140-6736(17)32464-9
Weiler, A. M., Hergesheimer, C., Brisbois, B., Wittman, H., Yassi, A., & Spiegel, J. M. (2015). Food sovereignty, food security and health equity: A meta-narrative mapping exercise. Health Policy and Planning, 30(8), 1078–1092. https://doi.org/10.1093/heapol/czu109
Wilson, K., von Tigerstrom, B., & McDougall, C. (2008). Protecting global health security through the International Health Regulations: Requirements and challenges. Canadian Medical Association Journal, 179(1), 44–48. https://doi.org/10.1503/cmaj.080516
World Health Organization. (1948). Preamble. In WHO, Constitution of the World Health Organization (pp. 1–2). https://apps.who.int/gb/bd/PDF/bd47/EN/constitution-en.pdf?ua=1
WHO. (1986). The Ottawa Charter for Health Promotion. https://www.who.int/healthpromotion/conferences/previous/ottawa/en/
WHO. (2016). Building health security beyond Ebola: Report of a high-level meeting. https://apps.who.int/iris/bitstream/handle/10665/250133/WHO-HSE-GCR-2016.13-eng.pdf
World Wildlife Fund. (n.d.). Deforestation and forest degradation. https://www.worldwildlife.org/threats/deforestation-and-forest-degradation
Worsnop, C. Z. (2019). The disease outbreak–human trafficking connection: A missed opportunity. Health Security, 17(3), 181–192. https://doi.org/10.1089/hs.2018.0134
Yeudall, F., Sebastian, R., Cole, D. C., Ibrahim, S., Lubowa, A., & Kikafunda, J. (2007). Food and nutritional security of children of urban farmers in Kampala, Uganda. Food and Nutrition Bulletin, 28(2, Suppl. 2), S237–S246. https://doi.org/10.1177/15648265070282S203
Young, O. R. (2013). The sustainability transition: Governing coupled human/natural systems. In G. Hoogensen Gjørv, D. Bazely, M. Goloviznina, & A. Tanentzap, (Eds.), Environmental and human security in the Arctic (pp. 83–97). Routledge.
Zimmerman, C., Kiss, L., & Hossain, M. (2011). Migration and health: A framework for 21st century policy-making. PLOS Medicine, 8(5), Article e1001034. https://doi.org/10.1371/journal.pmed.1001034
Long Descriptions
Figure 17.1 long description: Graphic composed of three layers of ovals enclosing each other. The outermost oval is labelled “Macro social, political, economic and ecological context of resource development projects.”
The second oval reads “industry-related pressures to social, economic, cultural and ecological processes” and “interactions with past, present and future land uses.”
The third and innermost oval is labelled “resulting and interralated changes to local context.” This oval contains four boxes that detail the determinants of health in the areas of social, environmental (or ecological), cultural, and economic change. They are described in an unordered list below:
- Social determinants of health
- Infrastructure/services
- Demographics and migration
- Social relationships
- Crime and safety
- Family dynamics
- Education
- Lifestyles
- Traffic
- Racial/ethnic impacts
- Gender impacts
- Food security
- Ecological determinants of health
- Noise
- Air quality
- Water quantity/quality
- Soil and sediment
- Climate change
- Landscapes
- Biodiversity
- Ecosystem services
- Geomorphology
- Wildlife health
- Cultural determinants of health
- Cultural practices
- Connection to culture
- Self-determination
- Local, traditional foods and medicines
- Connections to lands/waters
- Language use
- Intergenerational impacts
- Economic determinants of health
- Income and income distribution
- Economic systems
- Cost of living
- Poverty
- Housing
- Community investment
There is a fifth box that partially overlaps the four others. It is labelled “Health Impact Areas” and contains the following:
- Mental health
- Injuries
- Communicable diseases
- Substance use and related harms
- Sexual health
- Health behaviours
- Chronic and acute illness
- Health equity
Figure 17.2 long description: Map labelled “Northern British Columbia Overview: Change in industrial land-use.” The map shows approximately the most northerly two-thirds of British Columbia, including the islands of Haida Gwaii to the west and a small section of the eastern border with the Rocky Mountains and Alberta. This map was created in July 2018 for the Cumulative Impacts Research Consortium in Prince George.
The map shows that the northeastern section of the province, from the corner to the area approximately Fort St. John, saw a lot of industrial activity pre-2006. The central part of the province, radiating outward from Prince George, also saw significant industrial activity pre-2006. Along a few key pathways in the province, where a number of towns and First Nations communities are clustered, there has been industrial activity from 2006 to the present.
Figure 17.3 long description: Circular chart titled “Reciprocal relationships between the health of humans, animals and ecosystems.” In the centre of the circle is a three-piece pie chart that is surrounded by bubbles describing various health concerns. The pieces of the pie chart are at the top level of the following unordered list, while the bubbles are described in the sub-bullets:
- Equity/power/justice
- Political ecology of health
- Environmental health justice
- Ecohealth
- Nested ecological scales
- Ecohealth
- Ecological public health
- Planetary health
- Host/vector interaction
- Occupational environmental health
- One health
Media Attributions
- Figure 17.1 © 2019 Chris Buse is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Figure 17.2 © 2019 Chris Buse is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Figure 17.3 © 2018 Chris Buse adapted by Chris Buse (2019) is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Adapted from Aldis, 2008, pp. 371–372 ↵
The activities that may minimize risks or impacts of acute events on the collective health of a population living within a defined region (Chapter 17).
There are many debated definitions (Carr, 2015), but the classic is “A livelihood comprises the capabilities, assets (including both material and social resources) and activities for a means of living. A livelihood is sustainable when it can cope with and recover from stresses and shocks, maintain or enhance its capabilities and assets, while not undermining the natural resource base” (Chambers & Conway, 1992, p. 6) (Chapter 17).
Largely applied to agricultural practices, it refers to preventative measures designed to mitigate or reduce the risks associated with transmitting infectious disease to humans from other living organisms (e.g., crops, livestock, invasive species, pests), later broadened to include an array of harmful biological agents including chemical compounds (Chapter 17).
A system that represents both biogeophysical units and social actors and institutions (Chapter 17).
The benefits humanity obtains from ecosystems. These include provisioning services such as food and water; regulating services such as regulation of floods, drought, land degradation, and disease; supporting services such as soil formation and nutrient cycling; and cultural services such as recreational, spiritual, religious and other nonmaterial benefits (Alcamo et al., 2003) (Chapter 3, Chapter 17).
The capacity of a population to safeguard sustainable access to adequate quantities of acceptable quality water for sustaining livelihoods, human well-being and socio-economic development, for ensuring protection against water-borne pollution and water-related disasters, and for preserving ecosystems in a climate of peace and political stability (UNU-INWEH, 2013) (Chapter 17).
Any intermediate scale that can be located between larger and smaller systems or scales (Chapter 17).
There are multiple potential definitions (Weiler et al., 2014). One, in relation to human security, is “Food security exists when all people, at all times, have physical, social and economic access to sufficient, safe and nutritious food which meets their dietary needs and food preferences for an active and healthy life” (FAO, 2016) (Chapter 17).
An ecologically and geographically defined area, or biogeographic unit, that is smaller than an ecozone, but larger than an ecoregion or an ecosystem. (See operationalization by Vilhena & Antonelli, 2015.) (Chapter 17)

