Pain and Mobility
10.7 Opioid Analgesics and Antagonists
Opioid analgesics are prescribed for moderate and severe pain. There are several types of opioids, and routes of administration that are listed in Table 10.7a ranging from use for moderate to severe pain.[1]
| Generic Name | Trade Name(s) | Route | Adult Dosage |
|---|---|---|---|
| morphine | MS Contin,
Statex M.O.S |
PO & Rectal
SubQ, IM, & IV |
30 mg (may be increased)
4-10 mg (may be increased) |
| codeine/acetaminophen | Tylenol #3 | PO | 30 mg/300 mg |
| fentanyl | Duragesic
Abstral |
Transdermal
IM IV |
12 mcg-100mcg/hr
0.5-1 mcg/kg 0.5-1 mcg/kg |
| hydromorphone | Dilaudid | PO
Rectal SubQ, IM & IV |
4-8 mg
3 mg 1.5 mg (may be increased) |
| oxycodone
|
Oxycontin
Percocet |
PO
PO |
5 mg-10 mg (may be increased)
5 mg/325 mg |
Opioids are delivered through a variety of routes. For instance, opioids are commonly used in patient controlled analgesia (PCA) including morphine, hydromorphone and fentanyl. To receive the opioid using a PCA device, the client pushes a button, which releases a specific dose but also has a lockout mechanism to prevent an overdose.[2]
Read more about opioid usage in Canada at this Health Canada website.
Table 10.7a also displays a medication card for several types of opioids including morphine, hydromorphone, and fentanyl.
Safety Considerations for Opioid Use
Selecting Opioid Routes and Drugs
It is important to consider that the type of opioid and their route have different effects on the client. For instance, hydromorphone is five times more potent than morphine. Fentanyl is 80-100 times more potent than morphine.[3]
The Opioid Crisis in Canada
Almost 25% of Canadians experience chronic pain and opioids have been commonly used for chronic pain management. Opioid prescriptions are also used for treating opioid dependence. However, there is debate about the effectiveness of treating chronic non-cancer pain with opioids based on concerns related to the safe usage of these medications.
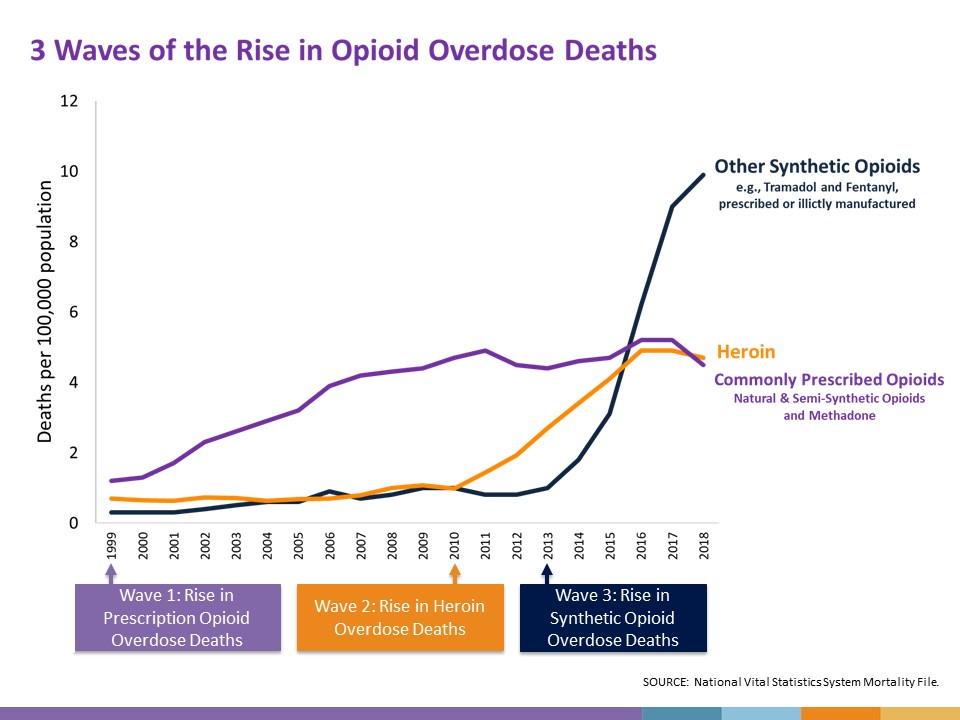
The past 30 years have seen waves of opioid-related deaths starting in the 1990s when overdose deaths were linked to a dramatic increase in prescription opioids for chronic pain. The wave increased again in 2010 when overdose deaths were more commonly related to illicit drug use.[4] Currently, most of the harm related to opioid use is due to the synthetic opioid, fentanyl, which is extremely potent and significantly increases the risk of overdose even in trace amounts. Figure 10.7a depicts the waves of opioid-related deaths in the United States, which closely mirrors the trend in Canada.[5]
From 2016 to 2019, there were more than 14,700 opioid-related deaths in Canada.[6] In 2016 in British Columbia, the provincial health officer declared a public health emergency under the Public Health Act due to the rise in opioid-related overdose deaths.[7]
In response to the public health emergency, the College of Physicians and Surgeons of British Columbia developed Professional Standards and Guidelines: Safe Prescribing of Drugs with Potential for Misuse/Diversion, based on the 2016 CDC Guideline for Prescribing Opioids for Chronic Pain.[8] Improving the prescription of opioids through clinical practice guidelines is intended to ensure clients have access to safer, effective pain treatment while also reducing the number of people who misuse or overdose from these drugs. In light of the overdose crises, is important for nurses to provide safe and equitable care for clients experiencing pain.
To learn more about substance use, refer to the British Columbia Center on Substance Use and the Canadian Center on Substance Use and Addiction.
Morphine Sulfate
Morphine is an opioid analgesic used to treat moderate to severe pain. Morphine is at the top of the WHO ladder and is used to treat severe pain. It is also commonly used to treat cancer pain and for pain at end of life because there is no “ceiling effect,” meaning the higher the dose, the higher the level of analgesia. The information provided below relates specifically to morphine, but can also be applied to other opioids such as hydromorphone and fentanyl.
Mechanism of Action
Morphine binds to opioid receptors in the CNS and alters the perception of and response to painful stimuli while producing generalized CNS depression.
Indications for Use
Morphine is indicated for the relief of moderate to severe acute and chronic pain and for pulmonary edema.
Nursing Considerations Across the Lifespan
Morphine can be used in all ages. It should be used cautiously in pregnant and breastfeeding women. Use cautiously with clients with liver and renal impairment. Elderly clients are more susceptible to toxic levels of opiates which can increase negative effects on the central nervous system, cardiovascular system, and gastrointestinal system.
Adverse/Side Effects
Adverse effects include respiratory depression, hypotension, light-headedness, dizziness, sedation, constipation, nausea, vomiting, sweating, and pruritis.
Client Teaching & Education
It is important to provide accurate information to clients about how to safely use opioids. This is especially true if clients are opiate naive. Additionally, clients might be worried about becoming addicted to opioids even with short-term usage. You can teach your client that most patients who use opioids do not become addicted.
Safety Warning
The risk of serious adverse reactions, including slowed or difficulty breathing and death, have been reported with the combined effects of morphine with other CNS depressants. Long-term usage of morphine may result in drug tolerance, dependence, and/or misuse. Naloxone is used to reverse opioid overdose.
Special Considerations
Respiratory Depression
Respiratory depression is the primary risk of morphine sulfate. Respiratory depression occurs more frequently in the elderly or those suffering from conditions accompanied by hypoxia, hypercapnia, or upper airway obstruction, for whom even moderate therapeutic doses may significantly decrease pulmonary ventilation.
Use morphine with extreme caution in clients with chronic obstructive pulmonary disease or cor pulmonale and in clients having a substantially decreased respiratory reserve, hypoxia, hypercapnia, or pre-existing respiratory depression. In such clients, even usual therapeutic doses of morphine sulfate may increase airway resistance and decrease respiratory drive to the point of apnea. Consider alternative non-opioid analgesics, and use morphine sulfate only under careful medical supervision at the lowest effective dose in such patients.
Misuse of Opioids
Morphine sulfate is an opioid agonist and is a controlled substance. Morphine can be used in a manner similar to other opioid agonists, legal or illicit. This should be considered when prescribing or dispensing morphine sulfate in situations where there is an increased risk of misuse.
Interactions with Alcohol and Drugs of Abuse
Morphine has addictive effects when used in conjunction with alcohol, other opioids, or illicit drugs that cause central nervous system depression because respiratory depression, hypotension, profound sedation, coma, or death may result.
Use In Head Injury and Increased Intracranial Pressure
In the presence of head injury, intracranial lesions, or a preexisting increase in intracranial pressure, the possible respiratory depressant effects of morphine and its potential to elevate cerebrospinal fluid pressure may be markedly exaggerated. Furthermore, morphine can produce effects on pupillary response and consciousness, which may obscure neurologic signs of increased intracranial pressure in clients with head injuries.
Hypotensive Effect
Morphine may cause severe hypotension in individuals unable to maintain blood pressure who have already been compromised by a depleted blood volume or drug administration of phenothiazines or general anesthetics. Administer morphine sulfate with caution to clients in circulatory shock, as vasodilation produced by the drug may further reduce cardiac output and blood pressure.
Gastrointestinal Effects
Do not administer morphine to clients with gastrointestinal obstruction, especially paralytic ileus because morphine diminishes propulsive peristaltic waves in the gastrointestinal tract and may prolong the obstruction. The administration of morphine sulfate may obscure the diagnosis or clinical course in clients with an acute abdominal condition.
Use in Pancreatic/Biliary Tract Disease
Use morphine with caution in clients with biliary tract disease, including acute pancreatitis, as morphine sulfate may cause spasming and diminished biliary and pancreatic secretions.
Special Risk Groups
Use morphine with caution and in reduced dosages in clients with severe renal or hepatic impairment, Addison’s disease, hypothyroidism, prostatic hypertrophy, or urethral stricture, and in elderly or debilitated clients. Exercise caution in the administration of morphine sulfate to clients with CNS depression, toxic psychosis, acute alcoholism, and delirium tremens. All opioids may aggravate convulsions in clients with convulsive disorders, and all opioids may induce or aggravate seizures.
Driving and Operating Machinery
Caution clients that morphine sulfate could impair the mental and/or physical abilities needed to perform potentially hazardous activities such as driving a car or operating machinery.
Caution clients about the potential combined effects of morphine sulfate with other CNS depressants, including other opioids, phenothiazines, sedative/hypnotics, and alcohol.
Opioid Analgesic Medication Card
Now let’s take a closer look at the medication card for opioid analgesics.[9] Medication cards like this are intended to assist students to learn key points about each medication. Because information about medication is constantly changing, nurses should always consult evidence-based resources to review current recommendations before administering specific medication. Basic information related to each class of medication is outlined below. Prototype or generic medication examples are also hyperlinked to a free resource at Daily Med. On the home page, enter the drug name in the search bar to read more about the medication.
Medication Card 10.7.1: Opioid Analgesic
Generic Name (Prototype/Brand Name):
morphine sulfate (M-ESlon, MS Contin)
hydromorphone (Dilaudid)
fentanyl (Duragesic)
Mechanism: Binds to opioid receptors in the CNS and alters the perception of and response to painful stimuli while producing generalized CNS depression.
Therapeutic Effects
- Treatment of moderate to severe pain
- Suppression of cough or respiratory distress
Administration
- IR and SR oral preparations
- IV, SC, IM, rectal, epidural, or transdermal.
- Used in all ages.
- Caution in pregnant and breastfeeding women, liver and renal impairment, and elderly clients.
- If nausea, take with food and lay quietly
Indications
- Relief of moderate to severe acute and chronic pain
- Analgesic during anesthesia
- Pulmonary edema
- Cancer pain and pain at end of life because there is no “ceiling effect,”
Contraindications
- Acute pancreatitis
- Renal impairment
- Liver impairment
- Respiratory depression
- Paralytic ileus
- Obstructive airway disease
- Increased intracranial pressure
- Acute alcoholism
Side Effects
- CNS depression (respiratory, CVS, sedation, N/V, sweating) respiratory depression
- Sweating, Pruritis
- Potentially Fatal: Respiratory depression; circulatory failure; hypotension; deepening coma; anaphylactic reactions.
- SAFETY Assess resp and sedation, naloxone for reversal. Consider a bowel regime for risk of constipation.
Nursing Considerations
- Assess for allergies, S&S of respiratory & CNS depression, GI obstruction, head injury etc.
- Do not perform hazardous activities
- No other CNS depressants.
- Do not cut, crush, or chew controlled release
- Dilute and administer IV slowly
Oral morphine was administered to a client for rib pain (rated as “6”) from metastatic lung cancer.
When should the effectiveness of the medication be evaluated?
Note: Answers to the Critical Thinking activities can be found in the “Answer Key” sections at the end of the book.
Opioid Antagonists
Naloxone
Naloxone is an opioid antagonist.
Mechanism of Action
Naloxone reverses analgesia and the CNS and respiratory depression caused by opioid agonists. It competes with opioid receptor sites in the brain and, thereby, prevents binding with receptors or displaces opioids already occupying receptor sites.
Indications for Use
Naloxone is indicated for the complete or partial reversal of opioid depression, including respiratory depression induced by natural and synthetic opioids.
Nursing Considerations Across the Lifespan
The safety and effectiveness of naloxone have not been established in children. Naloxone is contraindicated for pregnant and lactating women.
Adverse/Side Effects
Adverse effects include tremors, drowsiness, sweating, decreased respirations, hypertension, nausea, and vomiting. Clients may also experience acute narcotic abstinence syndrome. Additionally, if naloxone reverses an opioid that was indicated for pain, the pain may return.
Client Teaching & Education
Clients should be advised regarding the risks associated with opioid analgesic use. Clients and their families should be provided information about how to use opioid antagonists such as the information from BC Pharmacists. Clients may also be provided with a naloxone kit.
Special Considerations
Postoperative
The following adverse events have been associated with the use of naloxone hydrochloride injection in postoperative clients: hypotension, hypertension, ventricular tachycardia and fibrillation, dyspnea, pulmonary edema, and cardiac arrest. Death, coma, and encephalopathy have been reported as results of these events. Excessive doses of naloxone in postoperative clients may result in significant reversal of analgesia and may cause agitation.
Opioid Reversal
Abrupt reversal of opioid depression may result in nausea, vomiting, sweating, tachycardia, increased blood pressure, tremulousness, seizures, ventricular tachycardia and fibrillation, pulmonary edema, and cardiac arrest, which may result in death.
Opioid Dependence
Abrupt reversal of opioid effects in persons who are physically dependent on opioids may precipitate an acute withdrawal syndrome, which may include, but is not limited to, the following signs and symptoms: body aches, fever, sweating, runny nose, sneezing, piloerection, yawning, weakness, shivering or trembling, nervousness, restlessness or irritability, diarrhea, nausea or vomiting, abdominal cramps, increased blood pressure, and tachycardia. In the neonate, opioid withdrawal may also include convulsions, excessive crying, and hyperactive reflexes.
Naloxone Medication Card
Now let’s take a closer look at the medication card for naloxone[10]
Medication Card 10.7.2: Naloxone
Generic Name: naloxone
Prototype/Brand Name: Narcan
Mechanism: competes with opioid receptor sites in the brain and, thereby, prevents binding with receptors or displaces opioids already occupying receptor sites.
Therapeutic Effects
- Reversal of analgesia and CNS and respiratory depression caused by opioid agonists.
Administration
- Safety and effectiveness have not been established in children.
- Caution for pregnant and lactating women
- repeated doses PRN
- IV onset: 2 mins
- IM onset: 3-5 mins
- Metabolism: Liver
- Excretion: Kidney (urine)
Indications
- complete or partial reversal of opioid effects
Contraindications
- Allergy to narcotic antagonists.
- Pregnancy, lactation.
- Narcotic addiction.
- CV disease.
Side Effects
- CNS: agitation, reversal of analgesia
- CV: tachycardia, blood pressure changes, dysrhythmias, pulmonary edema
- Acute narcotic abstinence syndrome
- SAFETY: If providing naloxone for an overdose consider CPR as needed to support the client.
Nursing Considerations
- Assess for allergies, and S&S of MI
- Conduct baseline pain assessment
- Excessive doses in postop clients may result in significant reversal of analgesia and may cause cardiovascular events
- Provide comfort measures to help client cope with pain
A post-operative client just received naloxone for respiratory depression.
When should the client’s respiratory status be reassessed?
Note: Answers to the Critical Thinking activities can be found in the “Answer Key” sections at the end of the book
Image Description
Figure 10.7a Three Waves of Opioid Overdose Deaths image description
A line graph that depicts deaths per 100,000 population due to different types of opioids between 1999 and 2018.
- Commonly prescribed opioids (natural and semi-synthetic opiods and methadone): From 1999 to 2011, the death rate per 100,000 population steadily rises from 1 to 5. There is a slight dip after that but it rises again by 2016.
- Heroin: From 1999 to 2010, the death rate per 100,000 remains quite steady at around 1. From 2010 to 2016, the death rate rises steadily to just under 5 per 100,000., then it levels out.
- Other synthetic opioids (e.g., Tramadol and Fentanyl, prescribed or illicitly manufactured): From 1999 to 2013, the death rate per 100,000 remains quite steady at around 1. From 2013 to 2018, the death rate rises steeply to 10 per 100,000.
Below the graph, three waves are identified:
- Wave 1: Rise in prescription opioid overdose deaths started in 1999.
- Wave 2: Rise in heroin overdose deaths started in 2010.
- Wave 3: Rise in synthetic opioid overdose deaths started in 2013.
- Vallerand, A. & Sanoski, C. A. (2019). Davis’s Drug Guide for Nurses (16th ed.). F.A. Davis Company. ↵
- McCuistion, L., Vuljoin-DiMaggio, K., Winton, M, & Yeager, J. (2018). Pharmacology: A patient-centered nursing process approach. pp. 268-270, 324, 332. Elsevier. ↵
- UptoDate. (2021). Dose conversion guide for commonly used opioids. https://www.uptodate.com/contents/image?imageKey=PALC/111216 ↵
- Centers for Disease Control and Prevention. (2018, December 19). Opioid Overdose, Understanding the Epidemic. https://www.cdc.gov/drugoverdose/epidemic/index.html. ↵
- 3 Waves of the Rise of Opioid Overdose Deaths by National Vital Statics System, CDC is licensed under CC0. ↵
- Government of Canada. (2021). Opioid-related harms in Canada: Integrating Emergency Medical Service, hospitalization, and death data. https://www.canada.ca/en/health-canada/services/opioids/data-surveillance-research/integrating-emergency-medical-hospitalization-death-data.html. ↵
- Government of British Columbia. (2020). Statistical Reports on Deaths in British Columbia. https://www2.gov.bc.ca/gov/content/life-events/death/coroners-service/statistical-reports ↵
- CDC. (2016). CDC Guideline for Prescribing Opioids for Chronic Pain. https://www.cdc.gov/mmwr/volumes/65/rr/rr6501e1.htm ↵
- This work is a derivative of Daily Med by U.S. National Library of Medicine in the public domain. ↵
- This work is a derivative of Daily Med by U.S. National Library of Medicine in the public domain. ↵
Patient-controlled analgesia (PCA) is a type of pain management that lets the client decide when to get a dose of pain medicine (typically an opioid). To receive the opioid, the patient pushes a button on the PCA device, which releases a specific dose but also has a lockout mechanism to prevent an overdose.
The use of illegal drugs and/or the use of prescription drugs in a manner other than as directed by a doctor, such as use in greater amounts, more often, or longer than told to take a drug or using someone else’s prescription.

