Gas Exchange
5.4 Clinical Reasoning and Decision-Making related to Gas Exchange
Clinical Reasoning and Decision-Making Related to Gas Exchange
Clinical reasoning is a way that we think and process our knowledge, including what we have read or learned in the past, and apply it to the current context of what we are seeing right now in practice [1] Nurses make decisions all the time, and making decisions requires a complex thinking process. There are so many useful tools to be found online that can support your thinking through to clinical judgments. In the past, and still relevant, is the nursing process. We will utilize the nursing process as well as clinical judgment tools to help you clearly understand further respiratory drugs and their application in practice.
Now that we have reviewed the respiratory system and common respiratory disorders, let’s apply your knowledge to support the learning of the respiratory system and drugs related to gas exchange.
Assessment
Although there are numerous details to consider when administering medications, it is always important to first think about what you are giving and why.
First, let’s think of why? Recognizing Cues
Respiratory medications are often given to alleviate allergies or cold symptoms, or to decrease/eliminate shortness of breath (SOB). An important piece of your nursing assessment should be to assess the client’s respiratory status. The respiratory assessment includes observing the respiratory rate and quality of respirations (shallow, deep), obtaining a pulse oximetry reading, and auscultating lung sounds. Other pieces of the assessment include inspecting skin color, such as observing for pallor, or cyanosis, and determining if there is a cough or sputumpresent. If sputum is present, it should be assessed for color, odor, consistency, and amount (COCA).
Additional baseline information to collect prior to the administration of any respiratory medication includes any history of allergy or previous adverse drug response.
Interventions
Next, plan (refine your hypothesis), and take action.
Respiratory medications are available in many different formulations, such as nasal spray, inhalations, oral tablets or liquids, injections, or intravenous route, so it is always important to verify the correct route and anticipate the associated side effects. For example, inhalations deliver the required medicine or medicines directly to the lungs, which means the medicine(s) can act directly on the lung tissues, minimizing systemic side effects. On the other hand, intravenous medications are administered to act quickly, but can cause systemic side effects. Additionally, some products contain more than one medicine with different dosages (for example, inhalers that combine a long-acting bronchodilator with a glucocorticoid).
During the administration of respiratory medications, it is important to anticipate the expected outcome of the medication and any common side effects. For example, albuterol is a short acting Beta-2 agonist that is given for bronchodilation. The nurse should plan to perform a respiratory assessment before and after administration of albuterol to document the effectiveness of the medication, as well as monitor for tachycardia, a common side effect.
Additionally, the nurse should also ensure the proper use of the inhalers by the client. Observe the client self-administering the medication, and further instruct the client in proper use.[2]
Evaluation
Finally, evaluate the outcomes of your action.
It is important to always evaluate the client’s response to a medication. With respiratory medications, the nurse should assess decrease in allergy symptoms (cough, runny nose, tearing eyes) and any decrease in shortness of breath. The nurse should complete a respiratory assessment (respirations, pulse oximetry, and lung auscultation) before and after the medications have been administered and compare the results. If the symptoms are not improving or the clinical assessment is worsening, prompt intervention is required (such as notification of the health care provider for further orders) to prevent further clinical deterioration. Utilizing tools such as this concept map helps work through thinking like a nurse. This map in figure 5.4 is an example of what a concept map could look like. Your own design may vary so do not worry. You should now take time to explore what you have read and apply it visually.
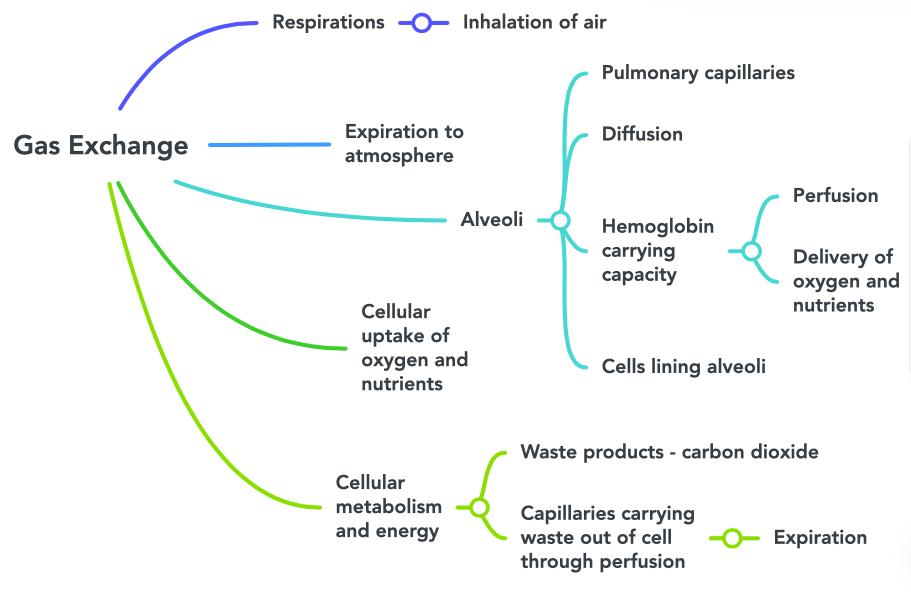
Image Description
Figure 5.4 Concept Map of Gas Exchange image description: This concept map illustrates the steps of gas exchange. The flow is as follows:
- Respirations
- Inhalation of air
- Expiration to atmosphere
- Alveoli
- Pulmonary capillaries
- Diffusion
- Hemoglobin carrying capacity
- Perfusion
- Delivery of oxygen and nutrients
- Cells lining alveoli
- Cellular uptake of oxygen and nutrients
- Cellular metabolism and energy
- Waste products – carbon dioxide
- Capillaries carrying waste out of cell through perfusion
- Expiration [Return to image]
- NCSBN. (n.d). NCSBN Clinical Judgement Measurement model. https://www.ncsbn.org/14798.htm ↵
- Drugs.com. (n.d.). Respiratory agents. https://www.drugs.com/drug-class/respiratory-agents.html ↵
A way that we think and process our knowledge including what we have read or learned in the past and apply it to the current practice context of what we are seeing right now.
A deficiency of color especially of the face: paleness.
Matter expectorated from the respiratory system and especially the lungs that is composed of mucus but may contain pus, blood, fibrin, or microorganisms (such as bacteria) in diseased states.

