Antimicrobials
3.13 Aminoglycosides
Aminoglycosides are potent broad-spectrum antibiotics that are useful for treating severe infections. Many aminoglycosides are poorly absorbed in the GI tract; therefore, the majority are given IV or IM. Aminoglycosides are potentially nephrotoxic and neurotoxic. They should be administered cautiously. Blood peak and trough levels should be performed to titrate a safe dose for each client.
Indications for Use: Streptomycin is used for streptococcal endocarditis and a second line treatment for tuberculosis. Neomycin is used in the treatment of hepatic encephalopathy as adjunct therapy to lower ammonia levels and is also used as a bowel prep for colon procedures.
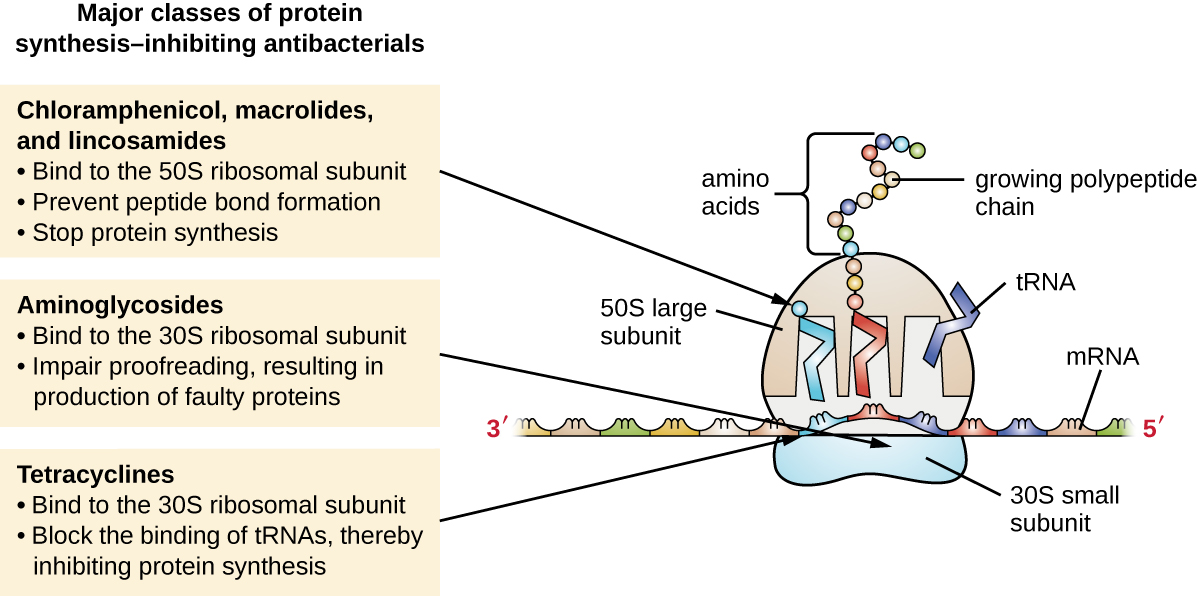
Mechanism of Action: Aminoglycosides are bactericidal and bind with the area of the ribosome known as the 30S subunit, inhibiting protein synthesis in the cell wall and resulting in bacterial death (see Figure 3.13).[1] Aminoglycosides may be given with beta-lactam medications to facilitate transport of aminoglycoside across the cellular membrane, resulting in a synergistic effect and increasing drug effectiveness.
Nursing Considerations Across the Lifespan: Aminoglycosides are safe to use in pediatric clients, with dose adjustments made based on the client’s weight. Some aminoglycosides are not safe for use in pregnancy, as they can cause fetal harm. In adult and older adult populations, renal function should be assessed as dose adjustments may be required.
Special Administration Considerations: Aminoglycosides can result in many adverse effects for the client and, therefore, the nurse should monitor the client carefully for signs of emerging concerns. Peak and trough levels are used to titrate this medication to a safe dose. Aminoglycosides can be nephrotoxic (damaging to kidney), neurotoxic (damaging to the nervous system), and ototoxic (damaging to the ear). Nurses should monitor the client receiving aminoglycosides for signs of decreased renal function such as declining urine output and increasing blood urea nitrogen (BUN), creatinine, and declining glomerular filtration rate (GFR). Indications of damage to the neurological system may be assessed as increasing peripheral numbness or tingling in the extremities. Additionally, the client should be carefully assessed for hearing loss or hearing changes throughout the course of drug administration.
ClientTeaching & Education: Clients receiving aminoglycosides should be advised to monitor for signs of hypersensitivity and auditory changes. This may include tinnitus and hearing loss. Clients may also experience accompanying vertigo while on the medication. Clients should be advised to drink plenty of fluids while taking the medication. Female clients should notify their provider if pregnancy is planned or if they are actively breastfeeding.[2]
Streptomycin and Gentamycin Medication Card
Now let’s take a closer look at the medication card for streptomycin and gentamycin.[3][4] Because information about medication is constantly changing, nurses should always consult evidence-based resources to review current recommendations before administering specific medication.
Medication Card 3.13.1: Aminoglycosides (streptomycin, gentamicin)
Class: Aminoglycosides
Prototypes: streptomycin, gentamicin
Mechanism: Bacteriocidal
Therapeutic Effects:
- Monitor for systemic signs of infection:
- WBC
- Temperature
- Culture results
- Monitor site of infection for improvement
Administration
- very potent
- never PO: poor absorption
- given w/B-lactams, vanco for synergy
- Gram –, some Gram +
- Exact mechanism not fully known, similar to tetracyclines
- Resistance can be overcome if used with penicillin or vancomycin
- Routes: IM, IV, topical
- inactivated by lactams (penicillins & cephalospirins) when coadmin to pts with renal insufficiency
Indications
- Serious Gram+ infections
- GI, GU
- Endocarditis
- Resp infections
Contraindications
- Preg/nursing: congenital deafness
- Allergy
- Renal impairment
- Loop diuretics
- Oral anticoagulants
Side Effects
- Ototoxicity (more common with pts taking furosemide)
- Nephrotoxicity
- Drug toxicity
- 8th cranial nerve damage = dizziness, nystagmus, vertigo, ataxia, tinnitus, roaring in ears, hearing impairment
- GI upset
- Rash
- Risk for severe neurotoxic reactions, especially with renal impairment. Can result in respiratory paralysis if given soon after anesthesia or muscle relaxant
- Can cause harm to fetus and breastfed infants
Nursing Considerations
- SEs most likely if pt: has hx of renal impairment, is dehydrated, getting high dosage, prolonged therapy, using other ototoxic drugs
- Renal assessment: proteinuria, BUN, creatinine
- Neuro assessment
- Hearing can come back after drug tx
- Report diarrhea immediately
Clinical Reasoning and Decision-Making Activity 3.13
Using the above grid information, consider the following clinical scenario question:
A client is admitted with streptococcal endocarditis and the nurse is preparing the morning dose of streptomycin. The lab test has not yet arrived to obtain the trough level, and the drug is now overdue to be given. What is the nurse’s next best response?
Note: Answers to the activities can be found in the “Answer Key” sections at the end of the book.
Image Description
Figure 3.13 Medications that inhibit protein synthesis: Diagram of a cell undergoing protein synthesis that describes the major classes of protein synthesis–inhibiting antibacterials. These include:
- Chloramphenicol, macrolides, and lincosamides, which:
- Bind to the 50S ribosomal subunit
- Prevent peptide bond formation
- Stop protein synthesis
- Aminoglycosides, which:
- Bind to the 30S ribosomal subunit
- Impair proofreading, resulting in production of faulty proteins
- Tetracyclines, which:
- Bind to the 30S ribosomal subunit
- Block the binding of tRNAs, thereby inhibiting protein synthesis
- This work is a derivative of Microbiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- uCentral from Unbound Medicine. https://www.unboundmedicine.com/ucentral ↵
- Daily Med, https://dailymed.nlm.nih.gov/dailymed/index.cfm, used for hyperlinked medications in this module. Retrieved June 27, 2019 ↵
- UpToDate (2021). Streptomycin. https://www.uptodate.com/contents/search ↵

