12.5 Medication Record and Documentation
Documentation
In addition to the documentation in the records and forms, including electronic systems, the client and team members involved in medication management should have an up-to-date list of all medications the client is taking, including prescription, over-the-counter (OTC), and alternative remedies/complementary medicine.
Medication Record
A medication administration record (MAR) is used by nurses and typically identifies individual medications and doses, including generic and trade names. When nurses administer medication, they are accountable for verifying that each medication administered matches the medication on the MAR, with space to sign each time it is provided to the client.
Health Care Assistants must also have a form or record to document the medication(s) they assisted with or administered (through client-specific delegation). As HCAs do not have training in pharmacology, they are not expected to have detailed knowledge of actions, interactions, contraindications, or indications of medication. By documenting in the medication record provided by the agency, the HCA acknowledges their participation in the medication care activity, confirms that the care activity was performed in accordance with the care plan and/or medication record, and provides written confirmation that it was completed at the specified date and time. The care plan and/or medication record provides any additional client-specific instructions, including the level of assistance the client may require.
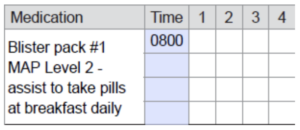
When an HCA documents on the medication record, a single signature and/or initial is required when assisting with a controlled dosage system that may contain single or multi-dose medication. See Figure 12.5.1.
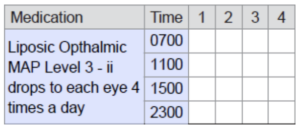
Each non-controlled dosage medication (e.g., a bottle of liquid eye drops or tube of prescription cream) also requires a signature and/or initial. Non-controlled dosage system medication should identify the name of the medication and additional direction as required such as route and/or specific location to be applied. See Figure 12.5.2.
Additional Medication Documentation Recommendations
The following recommendations promote standardized documentation for effective communication and client safety:
- Medication times should be identified using the 24-hour clock (e.g., 8:00 p.m. is recorded as 2000 hr.).
- Medication records must be available at the point of care for the HCA to perform required safety checks and the six rights of medication.
- Completion of the medication care activity shall be documented immediately after completion, at the point of care.
- Additional documentation is required when the client does not take medications as per the care plan, including the specific reason and follow-up action taken (e.g., Client refused morning medication. States “Blue pill upsets my stomach.” Supervisor and RN were notified (include the names of both).
- Documentation is only completed by the health care provider performing the activity and is never done on behalf of another health care provider.
- Documentation should be done for both the application and removal of transdermal patches.
- Track the site of application when medications, such as a transdermal patch, require rotating sites.
- When documenting in a paper-based systems:
- Use permanent blue or black ink; never write in pencil or use an eraser.
- Initials may be used to sign when the full name, signature, and initials are recorded on an employer maintained master signature record.
- Manage documentation errors according to employer policy, procedure or processes; never use white-out or felt markers to delete entries.
- Completed medication records should be retained with the client’s health record in accordance with employer policy and made available to the regulated health care provider accountable for care planning and medication reviews.
Reporting Errors
The RN who authorizes an HCA to perform a restricted activity (through client-specific delegation) is the primary contact person when concerns arise around the restricted activity or client. This remains true even at times when there are other RNs covering. The RN coordinates all aspects of the client support and any restricted activities that have been delegated to the HCA. Please note that social workers and LPNs are not able to delegate to HCAs. A site supervisor or manager is able to assist and support HCAs in training related to restricted activities, but only an RN may authorize the actual delegation. Additionally, the authorizing RN is responsible to ensure that individual HCA has the education, training, and competency to perform the restricted activity with that client. Please ask to speak to a RN when seeking urgent direction around any restricted activity.
Situations when the HCA should report an issue when assisting clients with medications may include:
- An issue with the controlled dosage system, such as:
- Wrong name is on pack.
- Client reports that the pills or number of pills are different from what is usually given.
- The pack has been tampered with and there is no explanation documented.
- The medication is not available or is past the expiry date or date range is incorrect.
- A possible medication error, such as:
- HCA forgot to give medication.
- HCA failed to follow one or more of the critical rights of medication.
- A pill was dropped in the sink or on the floor.
- Medication from previously scheduled doses found remaining in used blister bubble, such as:
- Medications were given to client from incorrect blister pack.
- A transdermal patch was not removed at correct time.
- Concerns regarding the client, such as:
- Client is ill.
- Client has vomited the medication.
- Client is refusing medication.
- Signs to observe that are noted on the care plan are present.
- Changed medication or requests for additional client assistance is not listed on the care plan or medication record, such as:
- New time for oral meds to be given.
- New medication in the home.
- Request from client/family to assist with medication.
- Other situations that arise that may be of concern to the HCA.
Medication errors do occur. If you think that you or someone else has made a medication error you must report this to the supervisor and RN so decisions on next steps can be made. Failing to report a medication error could result in losing your job and/or possible legal action. Reporting errors can help prevent harm to your client. When reporting medication errors, agency policies and procedures may require you to document either in the client’s chart and/or the completion of an incident form.
Summary
While medicines make a significant contribution to preventing and treating disease, increasing life expectancy, and improving quality of life, they also have the potential to cause harm. The inappropriate or incorrect use of medicines can have an adverse effect on the health of clients. Part of ensuring appropriate use is following instructions, protocols and guidelines. Health Care Assistants must understand their own roles and responsibilities and of those involved in medication management and follow the instructions, protocols, and guidelines in their role in providing assistance or administration.
Remember:
- HCAs may only administer medication under the direct supervision of a registered nurse.
- HCAs must never administer medication unless specifically delegated and trained to do so.
- HCAs are only able to administer the medications outlined in the HCA Program Provincial Curriculum 2023.
- HCA must adhere to procedures and requirements regarding medication assistance and administration that are outline by legislation, the HCA Program Provincial Curriculum and agency policies.
- HCAs can only participate in medications assistance or medication administration if they are over the age of 19.
- Who can authorize an HCA to perform a restricted activity like medication administration?
- Family members
- Physician
- Registered nurse (only RN can delegate to HCAs)
- All nurses and supervisors
- What kind of information always needs to be included on the client’s medication label?
- Client name
- Pharmacy name & phone number
- What route to be given
- All of the above
- If problems occur pertaining to a medication lockbox in the home, the HCA should call the:
- Supervisor
- Client’s family
- The last HCA who visited the client
- If the HCA has a concern about a restricted activity that has been delegated they should discuss the concern with the client or the family.
- True
- False (The HCA must discuss concerns with the regulated health professional who delegated the restricted activity.)
- An HCA should follow the the 6 six critical rights of medication administration?
- When the client is unfamiliar
- There has been a change on the care plan
- Every time you the HCA assists with or administer medications (The HCA is accountable for ensuring the right client, right medication, right time & day, right route, and right documentation is followed every time)
- There are some things that may make the HCA suspicious that the medication in the blister pack they are about to use may be incorrect. What are they?
- Client states these are the wrong pills
- Blister pack has been opened or tampered with and no corrective notation on it
- Names or dates are missing
- All of the above (All of these are indicators that HCA should what they are doing stop and seek direction.
- When an HCA documents on the medication record, a single signature and/or initial is required when assisting with a controlled dosage system.
- True
- False
- If the HCA has read the care plan once, they don’t need to read it on future visits to the client’s home.
- True
- False. HCAs must read the HS Service Plan and care plan on every visit to the client’s home, as changes to the client’s service may occur at any time without the HCA being aware of them. Checking these documents carefully on every visit ensures safe and accurate care for both the client and HCA.
- When should the HCA should report an issue?
- A possible medication error
- Concerns regarding the client
- Issue with the controlled dosage system
- All of the above (any or all of these should be reported to the supervisor or nurse).
- When meeting a client for the first time, all HCAs must use two client identifiers to ensure they have the correct person. What are appropriate identifiers to use?
- Client name
- Date of birth
- Address
- All of above
Unit 12 Attributions and References
Unit 12.3 Image Attributions
- Figure 12.3.1 Six Rights of Medication by T. Christianson is licensed under a CC BY 4.0 licence.
Unit 12.4 Image Attributions
- Figure 12.4.1 Lock box by OpenClipart, SVG ID: 20711, on FreeSVG.org is in the public domain.
- Figure 12.4.2 Blister Pack by Sprinno, via Wikimedia Commons, is used under a CC BY-SA 3.0 licence.
- Figure 12.4.3 Pill box by NIAID, via Wikimedia Commons, is used under a CC BY 2.0 licence.
References
Interior Health. (2017). Community health worker medication competency program: Home support education. Used with permission from the Director, Home Support Transformation.
Alberta Health Services – Policy, Practice, Access & Case Management Provincial Seniors Health and Continuing Care (2022). Medication assistance program (MAP) manual. https://www.albertahealthservices.ca/assets/info/seniors/if-sen-map-program-in-alberta.pdf
Medication that does not require a prescription and is taken to treat minor health problems at home.
A variety of treatments and remedies used in addition to traditional Western medicine. They include herbal or natural products available over-the-counter, such as St. John’s Wort, ginseng, or melatonin.
When a regulated health professional (such as an RN) authorizes an unregulated care provider (such as an HCA) to perform a restricted activity. Delegation is required because the restricted activity is normally the responsibility of a regulated health care professional and, therefore, outside of the role and training of the unregulated care provider. Delegation must be client-specific and is limited by the boundaries permitted by legislation and the regulated health professional’s regulatory college.

