8.3 Positioning Clients in Bed
Positioning a client in bed is important for maintaining alignment and preventing pressure injury, foot drop, and contractures (Perry et al., 2018). Proper positioning is also vital for providing comfort for clients who are bedridden or who have decreased mobility related to a medical condition or treatment. When positioning a client in bed, supportive devices such as pillows, rolls, wedges, and blankets, along with re-positioning, can aid in providing comfort and safety (Perry et al., 2018).
Positioning a client in bed is a common procedure. There are various positions possible for clients in bed, which may be determined by their condition, preference, or treatment related to an illness. Table 8.3.1 identifies client positions in bed and a description for each.
| Position | Description |
|---|---|
| Supine position | Client lies flat on back. Additional supportive devices for under lower legs or head may be added for comfort.
 |
| Prone position | Client lies on stomach with head turned to the side.
 |
| Lateral (side lying) position | Client lies on the side of the body with the top leg over the bottom leg. This position helps relieve pressure on the coccyx.
 |
| Sim’s position | Client lies between supine and prone positions with legs flexed in front of the client. Arms should be comfortably placed beside the client, not underneath.
 |
| Fowler’s position | Client’s head of bed is placed at a 45-degree angle. Hips may or may not be flexed. This is a common position to provide client comfort and care.

|
| Semi-Fowler’s position | Client’s head of bed is placed at a 30-degree angle. This position is used for clients who have cardiac or respiratory conditions, and clients with a nasogastric tube and who have enteral nutrition.
 |
| Orthopneic or tripod position | Client sits at the side of the bed with head resting on an overbed table on top of several pillows. This position is used for clients with breathing difficulties.
 |
| Trendelenberg position | Place the head of the bed lower than the feet. This position is used in situations such as hypotension and medical emergencies. It helps promote venous return to major organs such as the head and heart.
 |
Moving a Client Up in Bed
When moving a client in bed, perform a point-of-care risk assessment prior to the procedure to determine the level of assistance required for optimal client care. If a client is unable to assist with repositioning in bed, follow the agency’s no-lifting policy regarding the use of mechanical lifts for complex and bariatric clients. See Checklist 8.3.1 for the steps to move a client up in bed.
Checklist 8.3.1: Moving a Client Up in Bed
Disclaimer: Always review and follow your agency policy regarding this specific skill.
Safety considerations:
- Perform hand hygiene.
- Check room for additional precautions.
- Introduce yourself to client.
- Listen and attend to client cues.
- Ensure client’s privacy and dignity.
- Complete a point-of-care risk assessment for safer client handling
- Ensure tubes and attachments are properly placed prior to the procedure to prevent accidental removal.
- Ensure client has a draw sheet and friction-reducing sheet on the bed prior to repositioning.
| STEP | ACTION | ADDITIONAL INFORMATION |
|---|---|---|
| 1. | Make sure an additional health care provider is available to help with the move. | This procedure requires two health care providers. |
| 2. | Explain to the client what will happen and how the client can help. | Doing this provides the client with an opportunity to ask questions and help with the positioning. |
| 3. | Complete a point-of-care risk assessment Checklist 8.2.1 of client’s ability to help with the positioning. | This step prevents injury to client and health care provider. |
| 4. | Raise bed to safe working height. The bed should be flat. Ensure brakes are applied. Health care providers stand on each side of the bed. | Principles of proper body mechanics help prevent MSI.
Safe working height is at waist level of the shortest health care provider. Leaving the head of bed elevated increases effort required and increases risk of MSI.  |
| 5. | Lay client in supine position; place pillow at the head of the bed and against the headboard. | This step protects the head from accidentally hitting the headboard during repositioning. |
| 6. | Stand between shoulders and hips of client with feet shoulder width apart. Weight will be shifted from back foot to front foot. | This keeps the heaviest part of the client closest to the centre of gravity of the health care providers.
 |
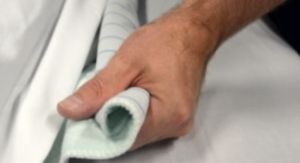
| 7. | Fan-fold the draw sheet toward the client with palms facing up. | This provides a strong grip to move the client up using the draw sheet.
 |
| 8. | Ask client to tilt head toward chest, fold arms across chest, and bend knees to assist with the movement. Let the client know when the move will happen. | This step prevents injury from client and prepares client for the move.
 |
| 9. | Tighten your gluteal and abdominal muscles, bend your knees, and keep back straight and neutral. | The principles of proper body mechanics help prevent injury. |
| 10. | On the count of three by the lead person, gently slide (not lift) the client up the bed, shifting your weight from the back foot to the front, keeping back straight with knees slightly bent. | The principles of proper body mechanics help prevent injury.
 |
| 11. | Replace pillow under head, position client in bed, and cover with sheets. | This step promotes comfort and prevents harm to client. |
| 12. | Lower bed, raise side rails as required, and ensure call bell is within reach. Perform hand hygiene. | Placing bed and side rails in safe positions reduces the likelihood of injury to client. Proper placement of call bell facilitates client’s ability to ask for assistance.
 Hand hygiene reduces the spread of microorganisms. |
Now complete the following online courses to learn more about how to move a client up in bed.
LearningHub is a province-wide course registry and learning management system for the health authorities in British Columbia. Sign up to learn more about moving clients in bed Slidersheet – Boosting & Turning – LearningHub (phsa.ca)
Positioning a Client to the Side of the Bed
Prior to ambulating, re-positioning, or transferring a client from one surface to another (e.g., a stretcher to a bed), it may be necessary to move the client to the side of the bed to avoid straining or excessive reaching by the health care provider. Positioning the client to the side of the bed also allows the health care provider to have the client as close as possible to the health care provider’s centre of gravity for optimal balance during client handling. Checklist 8.3.2 describes how to safely move a client to the side of the bed.
Checklist 8.3.2: Positioning a Client to the Side of the Bed
Disclaimer: Always review and follow your agency policy regarding this specific skill.
Safety considerations:
- Perform hand hygiene.
- Check room for additional precautions.
- Introduce yourself to client.
- Listen and attend to client cues.
- Ensure client’s privacy and dignity.
- Complete the point-of-care risk assessment (Checklist 8.2.1) for safer client handling
- Ensure tubes and attachments are properly placed prior to the procedure to prevent accidental removal.
- Ensure client has a draw sheet and a friction-reducing sheet on the bed prior to repositioning.
| STEP | ACTION | ADDITIONAL INFORMATION |
|---|---|---|
| 1. | Make sure you have as many additional health care providers as needed to help with the move. | The procedure works best with two or more health care providers, depending on the size of the client and the size of the health care professionals. |
| 2. | Explain to the client what will happen and how the client can help. | This provides the client with an opportunity to ask questions and help with the positioning. |
| 3. | Raise bed to safe working height and ensure that brakes are applied. Lay client in supine position. | Principles of proper body mechanics help prevent MSI.
Safe working height is at waist level of the shortest health care provider. |
| 4. | Stand on the side of the bed the client is moving toward.
One person stands at the shoulder area and the other person stands near the hip area, with feet shoulder width apart. |
This step keeps the heaviest part of the client closest to the centre of gravity of the health care providers.
 |
| 5. | Fanfold the draw sheet toward the client with palms facing up. |
 |
| 6. | Have the health care provider at the head of the bed grasp the pillow with one hand and the draw sheet with the other hand. | This prevents injury to client.
 |
| 7. | Have client place arms across chest. | This step prevents injury to client.
 |
| 8. | Tighten your gluteal and abdominal muscles, bend your knees, and keep back straight and neutral. Place one foot in front of the other. The weight will shift from the front foot to the back during the move. | Use of proper body mechanics helps prevent injury when handling clients.
|
| 9. | On the count of three by the lead person, with arms tight and shoulders down, shift your weight from the front foot to the back foot. Use your large leg muscles to move the client. Do not lift, but gently slide the client. |
  If the client is bariatric, the move should be repeated to correctly position the client or use a mechanical lift. |
| 10. | Once the client is positioned toward the side of the bed, ensure pillow is comfortable under the head, and straighten sheets. Complete all other procedures related to safe client handling. | This step promotes comfort and prevents harm to the client.
 |
| 11. | Lower bed, raise side rails as required, and ensure call bell is within reach. Perform hand hygiene. | Placing bed and side rails in safe positions reduces the likelihood of injury to client. Proper placement of call bell facilitates client’s ability to ask for assistance.
 Hand hygiene reduces the spread of microorganisms. |
LearningHub is a province-wide course registry and learning management system for the health authorities in British Columbia. Sign up to learn more about NHA – WHS – Safe Patient Handling: Patient Mobility Assessment – LearningHub (phsa.ca) While this course goes through the assessment of patient/client mobility, the video provides a good demonstration of positioning a patient/client to sit at the side of the bed.
Critical Thinking Exercises
- Your client is experiencing shortness of breath related to heart failure. Which position in bed might best help people with this condition?
- Consider how a mechanical assistive device might help with re-positioning a client in bed.
- Data sources: Perry et al., 2018; Potter et al., 2017. Images retrieved from 3.5 Positioning Patients in Bed in Clinical Procedures for Safer Patient Care by Glynda Rees Doyle and Jodie Anita McCutcheon, CC BY 4.0 ↵
- Data sources: Perry et al., 2018; PHSA, 2010. Images retrieved from 3.5 Positioning Patients in Bed in Clinical Procedures for Safer Patient Care by Glynda Rees Doyle and Jodie Anita McCutcheon, CC BY 4.0 ↵
- Data sources: Perry et al., 2018; PHSA, 2010. Images retrieved from 3.5 Positioning Patients in Bed in Clinical Procedures for Safer Patient Care by Glynda Rees Doyle and Jodie Anita McCutcheon, CC BY 4.0 ↵
The client sits at the side of the bed with head resting on an over-bed table on top of several pillows. This position is used for clients with breathing difficulties.
A policy that says health care providers are not to manually try to lift a client as this may result in serious injury to the client or care provider.

