9.9 Oxygen Saturation
What Is Oxygen Saturation?
Oxygen saturation refers to the percentage of hemoglobin molecules saturated with oxygen. Hemoglobin molecules can each carry four oxygen molecules; the oxygen binds or attaches to hemoglobin molecules. Oxygen saturation provides information about how much hemoglobin is carrying oxygen, compared to how much hemoglobin is not carrying oxygen.
Why Is Oxygen Saturation Measured?
Health care providers measure oxygen saturation because it provides information about a client’s state of health. The body’s tissues and organs require oxygen for metabolism, and oxygen saturation can reveal whether there is sufficient oxygen in the blood or whether the client is in a state called hypoxemia (insufficient oxygen in the blood).
Oxygen saturation levels can influence clinical decisions about whether the client is receiving sufficient oxygen and/or requires supplemental oxygen. Oxygen saturation levels are also monitored during and after surgeries and treatments and to assess a client’s capacity for increased activity.
How Is Oxygen Saturation Measured?
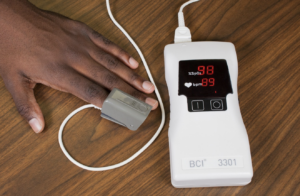
Oxygen saturation can be measured using a pulse oximetry device, which is a non-invasive method to measure arterial oxygen saturation level. There are various types of pulse oximeter devices. See Figure 9.9.1 for an example of a fingertip pulse oximeter.

A pulse oximetry device includes a sensor that measures light absorption of hemoglobin and represents arterial SpO2. Oxyhemoglobin and unoxygenated hemoglobin absorb light differently. The sensor measures “the relative amount of light absorbed by oxyhemoglobin and unoxygenated (reduced) hemoglobin” and compares the amount of “light emitted to light absorbed” (Jarvis, 2014, p. 164). This comparison is then converted to a ratio and is expressed as a percentage of Sp02.
The sensor is attached using various devices. One is a spring-loaded clip attached to a finger or toe as shown in Figure 9.9.2. It is used when an intermittent measurement is required.

What Are Normal Oxygen Saturation Levels?
The acceptable oxygen saturation range is 97–100%.
Older adults typically have lower oxygen saturation levels than younger adults. For example, someone older than 70 years of age may have an oxygen saturation level of about 95%, which is an acceptable level.
It is important to note that the oxygen saturation level varies considerably based on a person’s state of health. The Health Care Assistant’s role will be to measure oxygen saturation levels and report/record. The nurse will interpret the oxygen saturation levels. Listed below are conditions that may affect oxygen saturation levels:
- People who are obese or have conditions such as lung and cardiovascular diseases, emphysema, chronic obstructive pulmonary disease, congenital heart disease and sleep apnea tend to have lower oxygen saturation levels.
- Smoking can influence the accuracy of pulse oximetry in which the SpO2 is low or falsely high depending on whether hypercapnia is present. With hypercapnia, it is difficult for the pulse oximeter to differentiate oxygen in the blood from carbon monoxide (caused by smoking).
- Oxygen saturation levels may decrease slightly when a person is talking.
- Oxygen saturation may remain normal (e.g., 97% and higher) for people with anemia. However, this may not indicate adequate oxygenation because there are less hemoglobin to carry an adequate supply of oxygen for people who have anemia. The inadequate supply of oxygen may be more prominent during activity for people with anemia.
- Falsely low oxygen saturation levels may be associated with hypothermia, decreased peripheral perfusion, and cold extremities. In these cases, an ear lobe pulse oximeter device or arterial blood gases would provide a more accurate oxygen saturation level. However, arterial blood gases are usually only taken in critical care or emergency settings.
Oxygen Saturation Technique
The pulse oximeter probe is clipped onto or taped around a client’s finger, as shown in Figure 9.9.3. The device displays an oxygen saturation level and a pulse within a few seconds. Palpate the client’s radial pulse (taken for 30 seconds if regular and one minute if irregular) while the oximeter is attached to the finger. The health care provider can have confidence in the accuracy of the measurement of the oxygen saturation level if the pulse displayed on the oximeter coincides with the radial pulse.
The follow video demonstrates how to Measure Oxygen Saturation
Oxygen Saturation – Taken Correctly by Toronto Metropolitan University.
Points to Consider
Nail polish or artificial nails can interact with the absorption of light waves and influence the accuracy of the SpO2 measurement when using a probe clipped on the finger. Remove nail polish or use an alternative method.
Chapter Summary
Measuring oxygen saturation via pulse oximetry is a non-invasive way to quickly assess a client’s oxygen level. The Health Care Assistant’s role is to measure the oxygen saturation and report/record. The nurse is responsible for interpreting the oxygen saturation level and will consider the client’s health and wellness state, including any underlying conditions. There are various types of pulse oximeter devices available. Most often they will be attached to a finger or a toe.
Test Yourself
Now that you have completed this chapter, it’s time to test your knowledge. Try to answer the following questions.
- The acceptable oxygen saturation level is ______ % to _____ %.
- Match each person with the estimated SpO2 (95% SpO2, 97% SpO2, 92% SpO2).
- Health adolescent
- Adult with lung disease
- 80-year-old adult
- A client’s oxygen saturation is measured via pulse oximetry using a finger probe. The radial pulse does not coincide with the pulse displayed on the oximeter. How should the health care provider respond?
- Document the findings in the client’s chart.
- Repeat the measurements using an earlobe probe.
- Assume the client has hypoxic tissue injury.
- Notify the most responsible provider.
- The physician asks for an oxygen saturation report on a client who has peripheral limb tremors. Where is the best location to place the probe?
- Thumb
- Finger
- Ear
- Toe
- A person’s oxygen saturation is 89% and the pulse display on the pulse oximeter is aligned with the radial pulse. How should the Health Care Assistant respond?
- Give oxygen to the client.
- Ask the client, “Are you having any difficulty breathing?”
- Raise up the head of the client’s bed.
- Note this finding as normal and continue taking the vital signs.
- Organize the steps below in the correct order.
- Take radial pulse (30 seconds if regular and 1 minute if irregular).
- Clean oximeter probe with alcohol swab.
- Document or report findings.
- Turn pulse oximeter on.
- Clip or tape probe onto the client’s finger.
- Remove the client’s nail polish.
- Ensure radial pulse is aligned with pulse on the pulse oximeter.
- Which areas can a pulse oximeter sensor be attached on a person’s body? Select all that apply.
- Ankle
- Toe
- Forehead
- Neck
- Forearm
- Earlobe
- Finger
A protein found in red blood cells that combines with oxygen to carry to cells and tissues of the body.
The beat of the heart that is felt at an artery as blood passes through.

