7.3 Bowel Elimination
Normal Bowel Elimination
The stomach breaks down ingested food by means of stomach acid and enzymes. This product is called chyme. Chyme is passed into the small intestine through peristalsis. Chemical digestion and absorption of nutrients is the main function of the small intestine. The large intestine continues to absorb nutrients and fluid. The resulting waste is called feces and is stored in the colon and rectum until the urge to defecate is felt. The HCA should monitor the client’s bowel movements and note the frequency, consistency, colour, odour and any pain or discomfort experienced during bowel movements. This will assist the nurse in adjusting the client’s diet or medications.
Watch the video:
How Your Digestive System Works – Emma Bryce, from TED-Ed (2017).
Watch the video:
What is Peristalsis? by Mister Science (2018).
Characteristics of Normal Bowel Movements
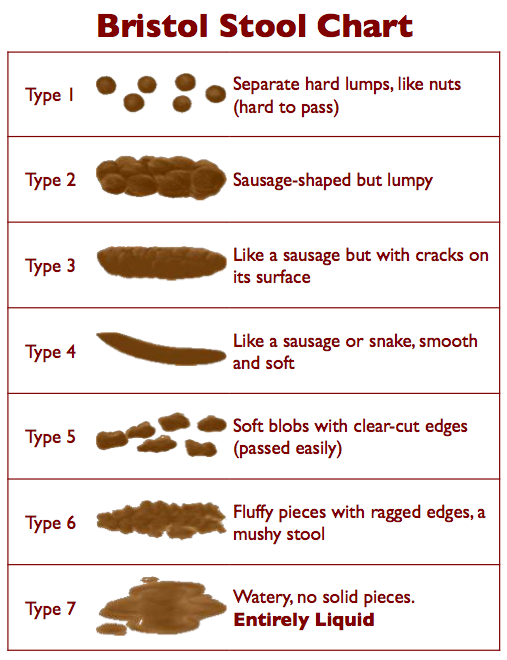
There is a range of normal when considering the frequency of bowel movements. It is important to know what is normal for your client. Some people have bowel movements daily, for others normal is every 2–3 days. The frequency of a person’s bowel movements can be affected by many factors, such as activity, age, medications, diet, fluid intake, and elimination habits. The Bristol Stool Chart (Figure 7.3.1) can assist you in identifying the consistency of the bowel movement.
| Characteristic: | What is Normal? |
| Colour | Normally brown due to presence of bile. |
| Amount | Normal can range from 3 times a day to 3 times a week. It is important to know what is normal for an individual, so changes can be identified. |
| Consistency | Normal is soft and formed. |
| Odour | Normal feces have a distinct odour. |
| Shape | Should be tube shaped, like the colon. |
| Size | Can vary depending on diet and elimination habits. |
| Pain or Discomfort | There should not be pain or discomfort felt with normal elimination. |
Abnormal Bowel Elimination
| Characteristic | Abnormal | Possible Causes |
|---|---|---|
| Colour | Black, red, green or other |
|
| Amount | Any increase or decrease from the client’s normal should be reported and monitored |
|
| Consistency/Shape | See Bristol Stool Chart (Figure 7.3.1) for variations in consistency/shape | Harder consistency can indicate lack of fluids/fibre in diet. Loose consistency can indicate infection, changes in diet, allergies or intolerances, or other disease processes. A thinner shape could indicate also indicate disease process. |
| Odour | Foul; different from usual stool | Foul or unusual odour can be the result of changes in diet, medications or infection |
| Size | Increase or decrease in normal should be monitored |
|
| Pain or Discomfort | Abdominal pain, cramping, rectal pain | Any pain or discomfort with defecation should be reported, as there are a variety of factors and causes. |
Assisting with Bowel Elimination
The Health Care Assistant plays an important role in assisting clients to maintain normal elimination patterns. By following the guidelines below, you can support independence and prevent constipation. Always ensure to check the care plan.
Guidelines for Assisting with Bowel Elimination
- Follow routine practices when assisting with elimination.
- Encourage fluids and appropriate fibre in diet as per the client’s care plan.
- Encourage exercise as appropriate.
- Provide assistance promptly. This is particularly important with the urge to defecate. If the client is not attended to promptly, the result may be that the urge goes away for several hours, contributing to constipation. The other result may be incontinence.
- Encourage clients to call when feeling the need to defecate.
- Provide for comfort and privacy as necessary.
- Ensure optimal positioning. If possible the client’s knees should be slightly higher than their hips.
- Utilize adaptive devices as per the care plan (raised toilet seat, mechanical lifts, commode, bedpan).
- Ensure safety of the client (provide the call bell and stand by if the client is unsteady).
- Provide peri-care after if the client is unable to do it themselves.
- Ensure to wash the client’s hands afterwards as well as your own.
- Record and report the time and amount of stool and anything abnormal to supervisor.
Problems with Bowel Elimination
Constipation
Constipation is a common problem experienced in older adults. Many factors contribute to constipation: age, medications, lack of adequate fluids or fibre, lack of exercise, delaying urge to defecate, lack of privacy. Frequent or constant constipation can lead to a variety of other health issues such as hemorrhoids, fecal impaction, and bowel obstruction. HCAs play an important role in preventing constipation in clients. Although prevention is key, HCAs may be involved in assisting with or caring for clients who have required other measures to address the constipation such as rectal suppositories, enemas or disimpaction.
Rectal suppositories and enemas are restricted activities taught in the HCA curriculum that an HCA could only perform if:
- It is delegated to the HCA by a regulated health professional (i.e., a registered nurse)
- It is delegated for a specific client
- The HCA performing the restricted activity is over the age of 19
- It is indicated in the client’s care plan
| STEP | ACTION | REASON |
|---|---|---|
| 1. | Check the client’s care plan. | Ensures you have information specific to this client’s care. |
| 2. | Perform hand hygiene before preparing supplies. | Following routine practices prevents the spread of pathogens. |
| 3. | Assemble equipment and supplies:
|
|
| 4. | Explain the procedure to the client. If client prefers to self-administer the suppository/enema, give specific instructions to client on correct procedure. |
|
| 5. | Raise bed to working height.
|
|
| 6. | Apply clean, non-sterile gloves. |
 Gloves protect the HCA from contact with mucous membranes and body fluids. |
| 7. |
|
|
| 8. |
|
|
| 9. |
|
|
| 10. | Remove finger and wipe client’s anal area. | Wiping removes excess lubricant and provides comfort to the client. |
| 11. | Ask the client to remain on side for 5–10 minutes. | This position helps prevent the expulsion of suppository. |
| 12. |
|
Using gloves reduces transfer of microorganisms.
  |
| 13. |
|
If suppository is a laxative or stool softener, client will require a bedpan/commode or close proximity to toilet.
 |
| 14. | Document procedure as per agency policy and include client’s tolerance of administration. | Timely and accurate documentation promotes client safety. |
Watch the video:
How to Give a Suppository orEnema, by CareChannel (2019).
Watch the video:
Perineal Care and Brief Change, by University of Manitoba Nursing Skills (2018).
Image Descriptions
Figure 7.3.1 Bristol Stool Chart
- Type 1 – separate hard lumps, like nuts (hard to pass)
- Type 2 – sausage-shape but lumpy
- Type 3 – like a sausage but with cracks on its surface
- Type 4 – like a sausage or snakes, smooth and soft
- Type 5 – soft blobs with clear-cut edges (passed easily)
- Type 6 – fluffy pieces with ragged edges, a mushy stool
- Type 7 – watery, no solid pieces, entirely liquid
- (Data sources: BCIT, 2015; Lilley, et al., 2016; Perry, et al., 2018) ↵
Muscular contractions of the gastrointestinal (GI) tract.
Body waste material discharged through the anus.
The process of eliminating waste from the digestive tract.
Condition in which a person has delayed or infrequent bowel movements, and the stool is hard, dry, and difficult to pass.
Hard, dry stool that stays in the rectum.



