13.2 Hot and Cold Applications: The Role of the HCA
Heat and cold applications offer comfort by reducing tissue swelling and promote healing. They are ordered to relieve pain, fight local infection, reduce swelling or inflammation, control bleeding, and reduce body temperature (Acello & Hegner, 2021). Regulated health care professionals (nurses, physiotherapists, and physicians) use heat and cold applications to reduce tissue swelling and promote healing and comfort for injuries and post-operations. Even though heat and cold are effective interventions, there are associated risks. Therefore, hot and cold applications should only be used if it is part of the client’s care plan if the task has been assigned to you by the nurse, and they should only be used for a specific length of time. Some facilities allow only regulated health professionals (i.e., nurses) to apply heat and cold, so be sure to follow the agency policies.
Hot and Cold Effects
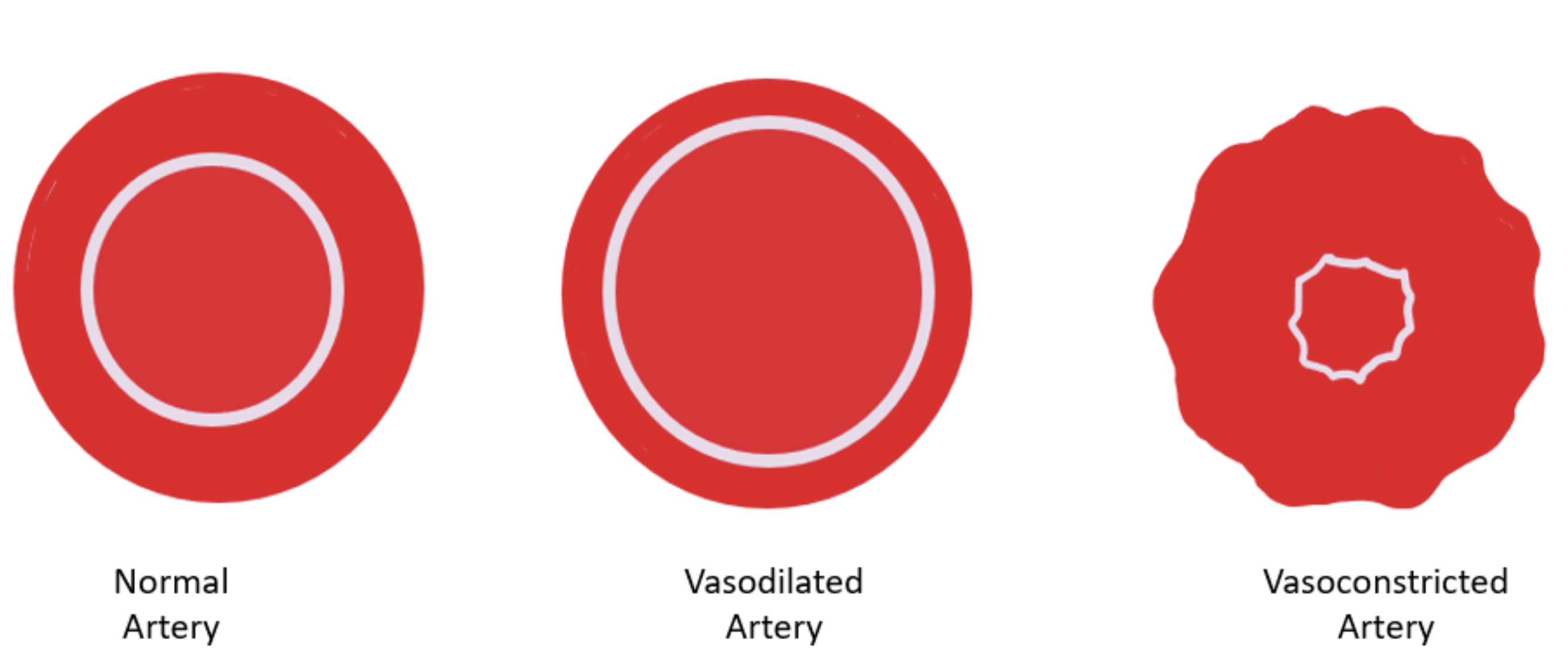
Think back to a time when you were really hot and you started sweating and your fingers were swollen. Now think about a time when you were really cold and you started to shiver and maybe your lips turned a little blue. What you experienced are the effects of heat and cold. Heat and cold have opposite effects on body functions. Heat increases blood flow by vasodilating blood vessels. When heat is applied to an area, the blood vessels in that area will dilate to increase blood flow. However, when cold blood flow is slowed by vasoconstricting blood vessels to conserve body heat. Applying a cold pack to an area will constrict blood flow in that area to reduce swelling. Figure 13.2.1 shows how an artery changes when it is vasodilated or vasoconstricted.
Heat Applications
Heat relieves pain, relaxes muscles, promotes healing, reduces tissue swelling, and decreases joint stiffness. When heat is applied to the skin blood vessels in the area dilate. Blood flow increases bringing more oxygen and nutrients to the surrounding tissue for healing. The vasodilation allows for excess fluid to be removed from the area faster. On observation, the skin will be red and warm to the touch (Acello & Hegner, 2021; Sorrentino, et al., 2019). Heat applications are also comforting. And the sensation of heat may decrease the transmission of pain signals to the brain which can relieve pain and discomfort. In addition, heat applications relax muscles and joints and this can decrease stiffness. Heat applications are used for chronic, or ongoing, conditions. These include back pain and arthritis. Heat applications may also be used only after the first two to three days following an acute, or sudden, injury (Acello & Hegner, 2021).
There are two types of heat applications: dry and moist. Dry heat applications are dry against the skin and no water touches the skin. Dry heat applications include hot packs, hot water bags, heating pads, and hot aquathermia pads. A dry application stays at the desired temperature longer. Moist heat applications are moist against the skin where the moisture or water touches the skin. Moist heat applications include hot compresses, hot soaks, and sitz baths. Moist heat applications Moist heat has greater and faster effects and are more penetrating than dry heat applications (Acello & Hegner, 2021; Sorrentino, et al., 2019).
Complications
High temperatures can cause burns. When heat is applied for too long, blood vessels will start to constrict. Persons at risk for complications include older adults, fair-skinned persons, those with decreased sensation to heat and pain. Persons with dementia and those who have metal implants are also at risk for injury. Others at risk for complications include:
- Loss of consciousness
- Scarring of the skin
- Use of some medications
- Spinal cord injuries
- Stroke
- Diabetes
- Aging
- Clients with dementia or cognitive impairment
- Clients with metal implants (pacemaker, joint replacement)
For temperature guidelines for hot applications, see Table 13.2.1 below.
Cold Applications
Cold applications are used for acute or sudden injuries, such as treat sprains, fractures, or fevers, and are therefore useful right after an injury. Cold applications have a numbing effect, so they relieve or reduce pain. When the blood vessels vasoconstrict, less blood is able to flow to the area. This in turn, decreases bleeding and reduces swelling. Cold is applied during the first two to three days following an injury.
There are two types of cold applications: dry and moist. Dry cold applications are dry against the skin and no water touches the skin. Dry cold applications include cold packs, ice bags, and cold aquathermia pads. Moist heat applications are moist against the skin where the moisture or water touches the skin. Moist cold applications include cold compresses and cold soaks. Moist cold applications are more penetrating than dry cold applications (Acello & Hegner, 2021; Sorrentino, et al., 2019).
Complications
Cold temperature can cause burns, pain, blisters, and poor circulation (See Table 13.2.1.) When cold is applied for a long time, blood vessels dilate as the body tries to warm the body temperature. Persons at risk for complications include older adults, fair-skinned people, and those with decreased sensation to heat and pain. People with dementia and those who have metal implants are also at risk for injury. Others at risk for complications include:
- Loss of consciousness
- Scarring of the skin
- Use of some medications
- Spinal cord injuries
- Stroke
- Diabetes
- Aging, which can cause decreased sensations due to changes in body function
- Clients with dementia or confusion
- Clients with metal implants (pacemaker, joint replacement)
For temperature guidelines for cold applications, see Table 13.2.1 below.
Remember:
Follow the agency guidelines for all hot and cold applications.
| Type of Application | Temperature in Celsius | Temperature in Farenheit |
|---|---|---|
| Hot | 37.7°C–40.5°C | 100°F–105°F |
| Warm | 35°C–37.7°C | 95°F–100°F |
| Tepid | 26.6°C–35°C | 80°F–95°F |
| Cool | 8.3°C–26.6°C | 65°F–80°F |
| Cold | 0°C–8.3°C | 50°F–65°F |
- To convert Fahrenheit to Celsius: C = (F − 32) × 5⁄9
- To convert Celsius to Fahrenheit: F = (C × 5⁄9) + 32
Hypothermia and Hyperthermia
Hypothermia is when the core body temperature drops below 35°C. While hyperthermia is when the core body temperature is excessively higher than normal. Under normal circumstances, the body is able to maintain its core body temperature within 1°C of 37°C. These excessively high or low body temperatures are managed and treated in acute care facilities. Hypothermia-hyperthermia blankets (aquathermia blankets) are placed over and under the clients to maintain temperature regardless of changes in the client’s body temperature. The health care team monitors the client’s temperature through a rectal, skin, or esophageal probe with the goal to maintain body temperature (Acello & Hegner, 2021).
Types of Applications
Aquathermia Pad (Aqua K-Pad)
An aquathermia pad is a pad with tubes inside. The pad is attached to a cooling/heating unit with two hoses. The cooling/heating unit is filled with distilled water to bring to desired temperature. The water flows through one of the hoses and into the tubes in the pad. Then the water flows through the other hose and back into the cooling/heating unit to maintain the desired water temperature before flowing back into the pad.

Cold Pack
A cold pack is a type of dry cold application. It is a pack that’s filled with cold fluid. Cold packs may be cooled by keeping them in the freezer, by striking or squeezing them to activate chemicals, or placing ice into bag or glove. The aquathermia pad can also be used as a cold pack. Cold packs are applied to the area of the body being treated. They may be reusable or disposable (Acello & Hegner, 2021; Sorrentino, et al., 2019).

Cold Compresses
A cold compress is a cloth or pad that is soaked in cold water. It is then applied to the area of the body being treated. A cold compress warms quickly so it must be resoaked and reapplied. Compresses such as 10 x 10 cm (4 × 4 inch) gauze pad or a Telfa pad, are used to apply moist cold to a small area. These compresses are easily made of washcloths or towels. Compresses and cold packs are usually not sterile. However, if there is a break in the client’s skin, sterile dressings may be used (Acello & Hegner, 2021; Sorrentino, et al., 2019).

Hot Pack
Hot packs can be hot water bags, heating pads, and hot aquamatic pads.Some hot packs are filled with hot fluid. Hot packs can be heated in the microwave, immersed in hot water, or activated by striking or squeezing to initiate a chemical reaction. Hot packs are applied to the area of the body being treated. They may be reusable or disposable. The water temperature of a hot pack should not exceed 43°C. A hot pack such as an electric heating pad or an aquathermia pad, which produces dry heat, is used to treat muscle sprains and mild inflammations and for pain relief. K-pads use temperature-controlled, distilled water that flows through the waterproof pad. The water temperature of a hot aquamatic pad is typically 35°C–41°C (Acello & Hegner, 2021; Sorrentino, et al., 2019).

Warm Compresses
Compresses, such as 10 x 10 cm (4 × 4 inch) gauze pad or a Telfa pad, are used to apply moist heat to a small area. Large warm, moist packs of cotton or terry cloth are used to apply heat over a larger area. Commercially prepared warm packs are also available and may be used to apply either dry or moist heat. Covering any hot pack with heavy, dry material helps it retain heat longer. Applying an Aqua-K pad over a hot pack enables the pack to remain heated almost indefinitely. The water temperature of a warm compress is typically 38°C–41°C. Compresses and hot packs are usually not sterile. However, if there is a break in the client’s skin, sterile dressings may be used (Acello & Hegner, 2021; Sorrentino, et al., 2019).

Hot Soak
A hot soak is a type of moist heat application that involves immersing the client’s affected body part in warm water or medicated solution for a prescribed time. The area of the body being treated is placed in a basin filled with hot water. The water temperature of a hot soak is typically 41°C– 49°C (Acello & Hegner, 2021; Sorrentino, et al., 2019).

Sitz Bath
A sitz bath is a type of moist heat application. The pelvic, perineal, and rectal areas of the body are placed in hot water. The water temperature of a sitz bath is typically 41°C. Disposable sitz basins are often used or a regular bathtub with enough water to cover the client’s hips and perineum (Acello & Hegner, 2021; Sorrentino, et al., 2019).
Role of an Assistant Health Care Assistants in Cold and Heat Applications
When performing cold and heat applications, HCAs must follow the client’s care plan. Specifically, HCAs need the following information:
- The area to be treated
- The type of application to be performed
- How to cover the application
- The temperature of the application
- How often to check the client
- How long to apply the application
In some health authorities and agencies, only physicians, therapists, and nurses may perform cold and heat applications. Health care assistants should only perform cold and heat applications if their agency permit them to do so. While performing a cold or heat application, HCAs must immediately report any problems to their supervisor. After performing a cold or heat application, HCAs must report and document all of the actions taken, including any observations and if the application resulted in pain relief, decreased stiffness, or reduced swelling.
Guidelines for Cold and Heat Applications
Any client receiving a heat or cold application should be frequently checked for any signs of problems related to their use. Inspect the skin beneath the application frequently, according to the care plan. It is advisable to check the skin every 5 minutes for the first two checks, and at least every 15 minutes after that (Sorrentino et al., 2013)). Because not every client may report having any discomfort, you should be particularly aware of signs such as restlessness, agitation, or other changes in behaviour. When performing cold and heat applications, HCAs must follow these guidelines (Acello & Hegner, 2021; Sorrentino, et al., 2019):
- Make sure the application is the temperature authorized in the client’s care plan.
- Never place an application directly on a client’s skin. Protect skin with a cloth as appropriate.
- Check the client frequently. If skin discoloration, swelling, or blisters occur, remove the application and tell the supervisor immediately.
- If clients complain of discomfort, pain, or numbness, remove the application and tell the supervisor immediately.
- If clients complain of weakness, dizziness, drowsiness, or faintness, remove the application and tell the supervisor immediately.
- Apply the application only for the amount of time authorized in the client’s care plan.
Because heat and cold applications produce different effects, HCAs must thoroughly understand the purposes, effects, and complications of these applications. There are risks involved, some employers allow only nurses to do the heat and cold applications. You, as the HCA, must be certain that this is within your role and the job description of the agency you work for.
Before you undertake the application of hot or cold therapies, it is your responsibility to make sure of the following (Sorrentino et al., 2013) :
- Your employer’s policies allow you to perform the procedure.
- The procedure is in your job description.
- You have been assigned to do so by a regulated health professional (i.e., RN).
- You have the necessary training.
- You are familiar with the equipment.
- You have reviewed the procedure with the RN.
- An RN is available to answer questions and to supervise you.
- You have confirmed what the temperature of the application should be and measured the temperature of moist applications before applying.
- Follow employer policies for safe temperature ranges. Do not apply hot applications above 41.1°C because tissue damage can occur. Only a nurse can apply a very hot application.
- Know the precise site of the application.
- Cover dry heat or cold applications with cloth before applying them. Use a flannel or terrycloth cover, towel, or pillowcase, according to your employer policy.
- Do not leave clients at risk unattended.
- Observe the client’s skin, at least every 5 minutes, for signs of complications
- Observe for changes in the client’s behaviour, which may indicate the client is in pain.
- Remind the client not to change the temperature of the application.
- Ask your supervisor how long to leave the application in place. Carefully watch the time. Heat and cold are applied for no longer than 15-minute periods.
- If it is safe to leave, place the call bell within the client’s reach, or remain within easy hearing distance.
Critical Reflection:
Situation: Mrs. Rosatti is 83 years old. This morning she twisted her ankle going to the bathroom. The nurse instructs you to apply a cold pack using ice to the area.
- How will you prepare the cold pack? Why is it important to remove excess air?
- How would you protect the skin from injury? Why is this important?
- How will you secure the cold pack in place?
- How often should you check the area? What signs and symptoms would you be observing for? What response would cause you to remove the pack?
- What would you tell Mrs. Rosatti if she asks why the ice must be removed after 20 minutes?
Summary
Hot and cold application have many benefits but if not performed correctly can cause injury. As a result, cold and heat applications must be performed correctly and physicians must order cold and heat applications for clients. Health care assistants may be able to support the health care team with such applications. However, the HCA must ensure that such tasks are within their role and they have received the appropriate training and support from the RN.
Chapter 13 Review Questions
- Which of the following is true about the area of heat application?
- It can reduce joint stiffness.
- It will treat recent sprains.
- It will cause an increase in muscle spasm.
- It will decrease the blood flow.
- Which of the following is the greatest threat from heat applications?
- Chilling
- Burns
- Infection
- Pressure ulcers
- Who has the greatest risk of complications from a heat application?
- A 10-year-old boy
- A 40-year-old woman
- A teenager
- An older adult with diabetes
- When checking the area of skin under a heat application, which of the following should you report?
- Rash
- Warm skin
- Client sleeping
- Relaxed muscles
- The temperature of a hot application is usually between:
- 33.8°C and 36.6°C
- 26.6°C and 33.8°C
- 41.1°C and 46.1°C
- 37.7°C and 40.5°C
- Which of these statements about moist heat applications is true?
- Moist heat has a greater and faster effect than dry heat
- Water is never in contact with the skin
- Heat applications are more dangerous than cold applications
- Dry heat penetrates deeper than moist heat
- A client has a warm compress. Which of the following is true?
- The warm compress is a dry heat application.
- The area is checked every 5 minutes.
- The compress should never be covered.
- The compress is applied no longer than 5 minutes.
- Cold applications:
- Dilate blood vessels
- Are warmed in a microwave oven
- Prevent the spread of microbes
- Reduce pain, prevent swelling, and decrease circulation
Chapter 13 Attributions & References
Image Attributions
- Figure 13.2.1: Artery Changes by T. Christianson is licensed under a CC BY 4.0 licence.
- Figure 13.2.2: Superficial Heat and Cold Applications in the Treatment of Knee Osteoarthritis | IntechOpen by Nurcan, C., & Karadağ, M. is licensed under a CC BY 3.0 licence.
- Figure 13.2.3: Ice pack by Dhenning2005, aka Dave Henning is in the Public domain.
- Figure 13.2.4: A Woman Putting Cold Compress on Her Face by Engin Akyurt is licensed under a Pexels License.
- Figure 13.2.5: Cold Hot Pack by Mamun2a, , via Wikimedia Commons, is licensed under a CC BY-SA 4.0 licence.
- Figure 13.2.6 Warm Compress by Neo139, via Wikimedia Commons, is licensed under a CC0 licence.
- Figure 13.2.8 Foot Soaking at a spa by Kolobetsoo, via Wikimedia Commons, is licensed under a CC BY-SA 4.0 licence.
- Figure 13.2.9 Sitz bath by loonyhiker is licensed under a CC BY-NC ND 2.0 licence.
References
Acello, B., & Hegner, B. (2021). Nursing Assistant: A Nursing Process Approach, 12th ed. Cengage.
Sorrentino, S., Remmert, L., & Wilks, M. (2019). Mosby’s Canadian textbook for the support worker (4th ed.).
To become enlarged, widened to open up blood flow.
To narrow the diameter of a blood vessel.
A condition in which the core body temperature drops below 35°C.
A condition in which the core body temperature is excessively higher than normal.
A pad that has tubes inside where water flows in and out of a heating/cooling unit.
A type of dry cold therapy used to reduce swelling and relieve pain. It consists of a pack filled with a cold substance, which can be cooled by various methods, such as freezing, chemical activation through squeezing or striking, or filling with ice.
A cloth or pad that is soaked in cold water. It is then applied to the area of the body being treated.
Packs used for heat therapy to relieve pain, relax muscles, and increase blood circulation. Examples include hot water bags or bottles, heating pads, and hot aquamatic pads.
A warm, shallow bath that a person sits in to relieve discomfort in the pelvic, perineal, and rectal areas.

