9.11 Weight and Height
Measuring Height and Weight
One of the tasks of the Health Care Assistant may be to measure the client’s height and weight on a regular basis. This helps to determine if the client is maintaining an adequate weight. Some clients may be on a special diet to lose weight, while others are prescribed diets to help them gain weight. Clients with conditions such as kidney or heart failure may have to be weighed on a daily basis to measure if the client is retaining fluid. Retaining fluid can lead to a worsening of their health condition.
Accuracy is important when weighing a client. Always ensure the scale is balanced to zero before weighing a client. When weighing a client, Health Care Assistants should encourage them to empty their bladder and bowels first. Weigh clients first thing in the morning and while they are wearing light clothing, such as pajamas. Shoes or slippers can also affect weight and height.
Depending on the client’s mobility, they may have a bed scale, chair scale, balance scale, or bathroom scale. Learn how to properly use each type of scale. It is important to ensure the safety of the client while weighing them. If a client appears unsteady and unable to stand in order to be weighed, inform the supervisor.
Remember too that people may be sensitive about their weight. Never chastise (scold) or be judgmental toward a person about their weight. Maintain privacy while weighing a client and do not disclose a client’s weight to others outside of the health care team, unless the client states it is okay.
Types of Scales
- Bed scale (the client is weighed while in bed)
- Chair scale (the client sits while being weighed)
- Balance scale (the type found in a doctor’s office)
- Bathroom scale (digital or standard)
| Step | Action | Rationale |
|---|---|---|
| 1 | Check the client’s care plan. | This ensures the HCA has accurate information about the client. |
| 2 | Explain the procedure to the client. | Clients have a right to information about their care. |
| 3 | Wash your hands. Don gloves as needed. | Following routine practices prevents the spread of pathogens. |
| 4 | Check that the scale is at “0”. Readjust if it is not. | This ensure the accuracy of the measurement. |
| 5 | Assist the client to the scale. | |
| 6 | Provide support while the client steadies themselves. | Ensures safety of the client. |
| 7 | Note the weight once the dial stops moving. | |
| 8 | Assist the client off the scale and safely back into a chair or bed. | |
| 9 | Wash hands. | Following routine practices prevents the spread of pathogens. |
| 10 | Record weight and any problems observed that the client may have had getting onto or off of the scale. | Timely and accurate documentation promotes client safety. |
| 11 | Report any changes in condition or behaviour (such as an increase or decrease in weight). | Timely and accurate documentation promotes client safety. |
| 12 | Store the scale in a safe place. | Ensures a clutter free, safe environment. |
| Step | Action | Rationale |
|---|---|---|
| 1 | Check the client’s care plan. | This ensures the HCA has accurate information about the client. |
| 2 | Explain the procedure to the client. | Client’s have a right to information about their care. |
| 3 | Wash your hands. Don gloves as needed. | Following routine practices prevents the spread of pathogens. |
| 4 | Gather Supplies needed: Measuring tape and ruler, notepad and pen | Organization ensures efficiency of procedure. |
| 5 | Assist the client into the supine position if able. | This ensures an accurate measurement. |
| 6 | Have an assistant hold the end of the measuring tape at the client’s heel. | This ensures an accurate measurement. |
| 7 | Pull the measuring tape alongside the client’s body until it extends past the head. | This helps measure the client’s height as if the person were standing. |
| 8 | Place the ruler flat across the top of the client’s head. It should extend from the client’s head to the measuring tape. Make sure the ruler is level. | If the ruler is not flat, the measurement will not be accurate. |
| 9 | Record the height on your notepad or assignment sheet. This ensures accurate recording of the height when transferring the information to the client’s record. | This ensures accurate recording of the height when transferring the information to the client’s record. |
| 10 | Ensure client is comfortable and provide call bell. | Ensures client safety. |
| 11 | Return equipment to proper location. | Ensures a clutter free, safe environment. |
| 12 | Wash hands. | Following routine practices prevents the spread of pathogens. |
| 13 | Report and record the height and your observations. | Timely and accurate documentation promotes client safety. |
Body mass index (BMI) is a standardized reference range that is used to analyze a client’s weight status and provides a representation of body fat. However, it is important to note that BMI may not be accurate for athletes with increased muscle mass, people with edema or dehydration, or older adults who have lost a significant amount of muscle mass. See a BMI table in Figure 9.11.1.
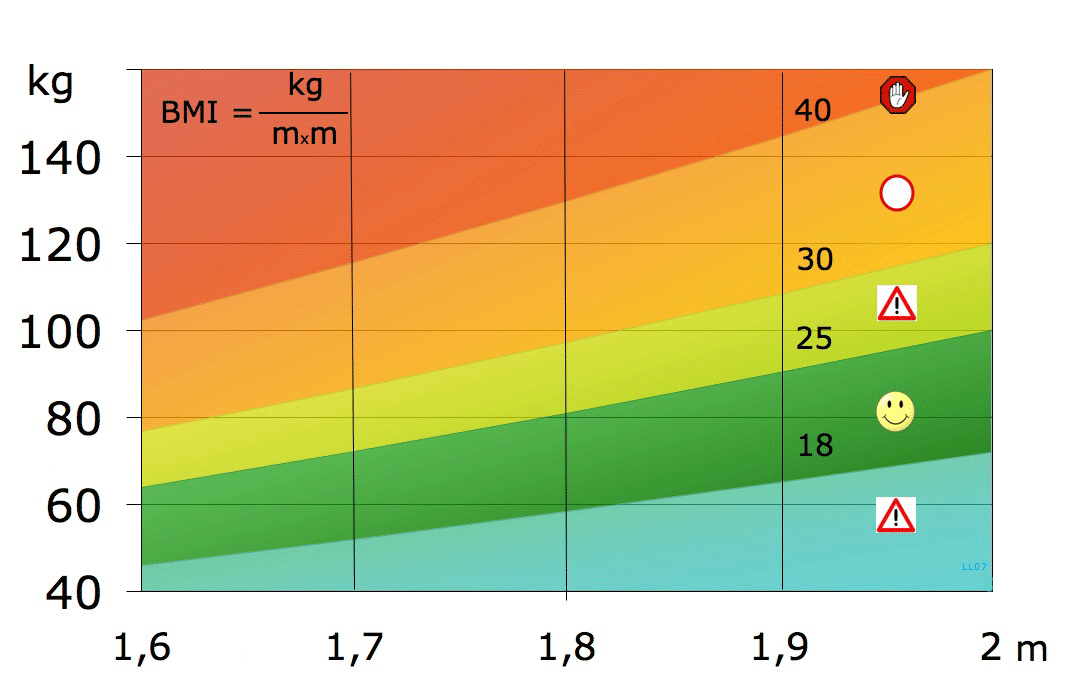
BMI can also be calculated using the formula of BMI = kg/m2 (weight in kilograms divided by height in meters squared).
The following classifications are used based on a person’s BMI:
- Underweight: Below 18.5 kg/m2
- Healthy weight: 18.6 to 24.9 kg/m2
- Overweight: 25 to 29.9 kg/m2
- Obesity: Over 30 kg/m2 to 34.9 kg/m2
- Extreme obesity: Over 35 kg/m2
Summary
Health Care Assistants play an important role on the health care team and can support nurses in the detection and monitoring of client’s health. The trained HCA can monitor, record, and report vital signs but must do these accurately because they provide critical information about the client’s condition. The administration of oxygen is a restricted activity, but HCAs may assist in caring for clients with oxygen.
Remember, when assisting with oxygen therapy and vital signs, it is important to understand what type of care activity is required to help the client meet their needs and whether that care activity is within your HCA role.
Chapter 9 Attributions and References
Unit 9.3
- Figure 9.3.1 Oxygen flow meter by Stephen Andrews is licensed under Pexels
- Figure 9.3.2 Portable oxygen tank by The U.S. food and Drug Administration is in the Public Domain
- Figure 9.3.3 Oxygen concentrator by BrokenSphere is licensed under CC BY-SA 3.0
- Figure 9.3.4 Applying a nasal cannula is retrieved from 5.6 Management of Hypoxia in Clinical Procedures for Safer Patient Care – TRU Edition by Renée Anderson, Glynda Rees Doyle, and Jodie Anita McCutcheon, CC BY 4.0.
- Figure 9.3.5 Nasal cannula by BruceBlaus is licensed under CC-BY-SA 4.0
- Figure 9.3.6 Simple face mask by James Heilman, MD is licensed under CC-BY-SA 4.0
- Figure 9.3.7 Non rebreather mask by James Heilman, MD is licensed under CC-BY-SA 4.0
- Figure 9.3.8 Face tent retrieved from 5.6 Management of Hypoxia in Clinical Procedures for Safer Patient Care – TRU Edition by Renée Anderson, Glynda Rees Doyle, and Jodie Anita McCutcheon, CC BY 4.0.
- Figure 9.3.9 Venturi mask from clinical procedures retrieved from 5.6 Management of Hypoxia in Clinical Procedures for Safer Patient Care – TRU Edition by Renée Anderson, Glynda Rees Doyle, and Jodie Anita McCutcheon, CC BY 4.0.
- Figure 9.3.10 Nebulizer by James Heilman, MD is licensed under CC-BY-SA 4.0
- Figure 9.3.11 High flow nasal cannula by Strangecow is licensed under CC0 1.0
Unit 9.4
- Figure 9.4.1 CPAP machine by myupchar is licensed under CC BY-SA 4.0
Unit 9.6
- Figure 9.6.1 Location of hypothalamus within the brain by BruceBlaus is licensed under CC BY-SA 4.0
- Figure 9.6.2 Oral thermometer is retrieved from Chapter 2. Temperature in Vital Sign Measurement Across the Lifespan – 2nd Canadian Edition by Jennifer L. Lapum, Margaret Verkuyl, Wendy Garcia, Oona St-Amant, and Andy Tan, CC BY 4.0.
- Figure 9.6.3 Oral temperature being taken is retrieved from Chapter 2. Temperature in Vital Sign Measurement Across the Lifespan – 2nd Canadian Edition by Jennifer L. Lapum, Margaret Verkuyl, Wendy Garcia, Oona St-Amant, and Andy Tan, CC BY 4.0.
- Figure 9.6.4 Tympanic thermometer is retrieved from Chapter 2. Temperature in Vital Sign Measurement Across the Lifespan – 2nd Canadian Edition by Jennifer L. Lapum, Margaret Verkuyl, Wendy Garcia, Oona St-Amant, and Andy Tan, CC BY 4.0.
- Figure 9.6.5 Tympanic temperature being taken is retrieved from Chapter 2. Temperature in Vital Sign Measurement Across the Lifespan – 2nd Canadian Edition by Jennifer L. Lapum, Margaret Verkuyl, Wendy Garcia, Oona St-Amant, and Andy Tan, CC BY 4.0.
- Figure 9.6.6 Axillary temperature being taken is retrieved from Chapter 2. Temperature in Vital Sign Measurement Across the Lifespan – 2nd Canadian Edition by Jennifer L. Lapum, Margaret Verkuyl, Wendy Garcia, Oona St-Amant, and Andy Tan, CC BY 4.0.
- Figure 9.6.7 Rectal thermometer is retrieved from Chapter 2. Temperature in Vital Sign Measurement Across the Lifespan – 2nd Canadian Edition by Jennifer L. Lapum, Margaret Verkuyl, Wendy Garcia, Oona St-Amant, and Andy Tan, CC BY 4.0.
Unit 9.7
- Figure 9.7.1 Radial, brachial, carotid and apical pulse. (Illustration credit: Hilary Tang)
- Figure 9.7.2 Correct placement of fingers retrieved from Radial Pulse in Vital Sign Measurement Across the Lifespan – 2nd Canadian Edition by Jennifer L. Lapum, Margaret Verkuyl, Wendy Garcia, Oona St-Amant, and Andy Tan, CC BY 4.0.
Unit 9.8
- Figure 9.8.1 Tripod position after running by Rennet Stowe is licensed under CC BY 2.0 licence.
- Figure 9.8.2 Signs of respiratory distress. (Illustration credit: Paige Jones)
Unit 9.9
- Figure 9.9.1 A fingertip pulse oximeter by Thinkpaul is licensed under a CC BY-SA 3.0 Unported licence.
- Figure 9.9.2 Spring loaded pulse oximeter is retrieved from 11.3 Oxygenation Equipment in Nursing Skills by Open Resources for Nursing (Open RN), CC BY 4.0.
- Figure 9.9.3 Measuring oxygen saturation is retrieved from Oxygen Saturation Technique in Vital Sign Measurement Across the Lifespan – 2nd Canadian Edition by Jennifer L. Lapum, Margaret Verkuyl, Wendy Garcia, Oona St-Amant, and Andy Tan, CC BY 4.0.
Unit 9.10
- Figure 9.10.1 Varying blood pressure cuff sizes is retrieved from How is Blood Pressure Measured? in Vital Sign Measurement Across the Lifespan – 2nd Canadian Edition by Jennifer L. Lapum, Margaret Verkuyl, Wendy Garcia, Oona St-Amant, and Andy Tan, CC BY 4.0.
- Figure 9.10.2 Blood pressure cuff with a sphygmomanometer and a stethoscope is retrieved from How is Blood Pressure Measured? in Vital Sign Measurement Across the Lifespan – 2nd Canadian Edition by Jennifer L. Lapum, Margaret Verkuyl, Wendy Garcia, Oona St-Amant, and Andy Tan, CC BY 4.0.
- Figure 9.10.3 Automatic blood pressure cuff is retrieved from How is Blood Pressure Measured? in Vital Sign Measurement Across the Lifespan – 2nd Canadian Edition by Jennifer L. Lapum, Margaret Verkuyl, Wendy Garcia, Oona St-Amant, and Andy Tan, CC BY 4.0.
Unit 9.11
- Figure 9.11.1 Body Mass Index by Laurens van Lieshout is used under a CC BY-SA 3.0 license.
References
Fisher & Paykel Health Care. (2018). Optiflow™ provides respiratory support via nasal cannula. https://www.fphcare.com/nz/hospital/adult-respiratory/optiflow/mechanisms-of-action/.
Leduc, D., & Woods, S., (2017). Canadian Paediatric Society position statement: Temperature measurement in paediatrics. http://www.cps.ca/en/documents/position/temperature-measurement
Mazerolle, S., Ganio, M., Casa, D., Vingren, J., & Klau, J. (2011). Is oral temperature an accurate measurement of deep body temperature? A systematic review. Journal of Athletic Training, 46(5), 566–573.
O’Driscoll, B. R., Howard, L. S., & Davison, A. G. (2008). Guideline for emergency oxygen use in adult patients. Thorax, 63(6). https://thorax.bmj.com/content/63/Suppl_6/vi1.
Perry, A. G., Potter, P. A., & Ostendorf, W. R. (2018). Clinical nursing skills & techniques (9th ed.). St. Louis: Elsevier-Mosby.
Wilk, M. (2022). Sorrentino’s Canadian textbook for the support worker. (5th Can. Ed).
Toronto, ON: Elsevier Canada
- (Data Source: Wilk, 2022). ↵

