Chapter 19. The Sociology of the Body: Health and Medicine
19.1 The Sociology of the Body and Health
Whereas human bodies have not changed radically since the evolution of Homo sapiens 200,000 years ago, humans’ relationship to their bodies has. Due to this change over the last 150 years — in biomedical knowledge, nutrition, hygiene, or sanitation, for example — people, on average, are healthier, taller, and live longer than their ancestors lived. In turn, these changes have had direct consequences for social organization.
Chapter 13. Aging and the Elderly discussed how the phenomenon of the aging population has forced governments, institutions, and individuals to rethink everything from pension plans, health care provisions, and mandatory retirement ages, to the bias towards youth in popular culture and marketing. As a political constituency, seniors are both significant in numbers and more engaged than young people. They are also healthier and live longer on average than previous generations of seniors. They can press the government to shift resources away from young people’s concerns to meet their own interests: for example, away from funding education to investing in medical research.
In his science fiction novel Holy Fire (1996), Bruce Sterling extrapolates from this phenomenon to imagine a future gerontocracy where seniors hold all the wealth and power, as well as the resources to invest in radical medical procedures, which extend their lives and health indefinitely. Young people are excluded from meaningful participation in society, and youth culture is no longer celebrated, but seen as reckless and irresponsible. The primary interest of the gerontocrats is their continued health, so their lifestyle involves a strict regimen of exercise, diet, avoidance of intoxicants, and aversion to risk. Sterling raises the question of a future epoch of post-humanity, i.e., a period in which the mortality that defined the human condition for millennia has effectively been eliminated through the technologies of life preservation.
Is this the postnatural future of humanity? How malleable is the human body? To what degree can it be redesigned to suit human purposes? In what way is the human body a sociological phenomenon as well as a physiological phenomenon?
The Sociology of the Body

Michel Foucault (1979) has argued that the shift in the way people related to their bodies in the 18th and 19th centuries is central to the formation of modern institutions and societies. In monastic practices, military discipline, factory organization, hospital design, prison rehabilitation, and educational programs, the individual body was redefined as something that needed to be trained, disciplined, and transformed. For the first time in history, the body became the center of numerous detailed procedures designed to improve its performance in a variety of institutional contexts. At the same time, the qualities of the life of the population as a whole came to be seen as a concern for government: public health, sanitary conditions in cities, the rate of population increase, and the need for a productive workforce, for example.
Foucault calls this the era of biopolitics: “the entry of life into history” or the moment when “the administration of bodies and the calculated management of life” became the priority in the organization of social life (Foucault, 1980). Authorities and individuals themselves began to seek ways to foster life and improve the body’s capacity for efficiency, health, learning, skills, and responsiveness. Today, preserving and fostering life might be the one central unifying value that underlies all contemporary politics and contemporary social policy concerns.
Foucault cites a military ordinance of 1764 with regard to the military training of recruits:
Recruits become accustomed to ‘holding their heads high and erect; to standing upright, without bending the back, to sticking out the belly, throwing out the chest and throwing back the shoulders; and, to help them acquire the habit, they are given this position while standing against a wall is such a way that the heels, the thighs, the waist and the shoulders touch it, as also do the backs of the hands, as one turns the arms outwards, without moving them away from the body . . . Likewise, they will be taught never to fix their eyes on the ground, but to look straight at those they pass . . . to remain motionless until the order is given, without moving the head, the hands or the feet . . . lastly to march with a bold step, with knee and ham taut, on the points of the feet, which should face outwards.’ (Foucault, 1979, pp. 135–136)
The military was one of the first institutions to take a detailed interest in training and modifying the human body. If before the 18th century, the individual’s body and the life of the population were matters of indifference to authorities, it is possible to argue that all institutional life after the 18th century became focused on disciplining and improving the individual body and collective life.
It is in this context that the concept of the norm became so important. A norm is a socially defined rule that distinguishes between what conforms to accepted standards and what does not. In the biopolitical era, norms are typically understood less as moral rules about what is morally correct or good and more based on calculated averages that define what is statistically normal behaviour or characteristic and what deviates from the norm (Ewald, 1990). In school, for example, norms define what level of knowledge each grade should attain. Within each grade level, students’ performance is judged in relationship to these norms, and as a result, they receive A, B, C, … . letter grades so they know where they stand academically with each other and with respect to normal expectations for their grade or age level. The whole learning operation depends on the detailed control of the students’ bodies and minds, as they must learn to physically read and write, sit quietly, listen to instruction, organize routines around a fixed schedule, and take steps to improve their abilities.
The same can be said about the norms of health in the medical system, the norms of productivity in the workplace, the norms of soldiering in the military, and the norms of “good behaviour” in the prison system. In each case, a disciplinary procedure is instituted to improve the individual’s abilities so that they can become normal (e.g., to enjoy normal health or work at a normal level of productivity). Therefore, regarding the establishment of norms, and what Foucault called the normalizing society, the problem of deviance became more prominent in the 19th and 20th centuries.
The problem of disabilities is a good example of medicalized deviance. Those with disabilities do not fit within the norms of the healthy body and therefore, beginning in the 19th century, scientists and reformers sought their rehabilitation through medical, technological, therapeutic, and educational interventions. This is discussed further below.
Today, the relationship to the body has become even more complex. People are still obliged by different institutions to act on their bodies in specific ways: to be more efficient at work, to recover from injury or illness through the health care system, to develop good study habits at school, and so on. However, people are also increasingly concerned about improving their bodies on a voluntary basis. Individually, people turn to experts in a variety of fields who advise them on different practices of the self or procedures to act upon their bodies, such as exercise regimes, dieting, cosmetic surgery, skin care products, meditation techniques, yoga, sex therapy, life coaching, and martial arts. A vast amount of information about life improvement and numerous competing options is available.
Increasingly modern societies enter an era of medical pluralism, in which no one model of health practice can successfully claim to provide the definitive truth for how to attain health. But as Zygmunt Bauman (2005) argues, the increased capacity people must control their bodies in the absence of certainty about which way is best, only increases their anxiety (2005). This is a key factor in contemporary debates about vaccines for example.
In addition, the control of the body has become increasingly “molecularized” through the advances of genetic and bio-chemical research (see Chapter 4. Society and Modern Life). That is, people attempt to act upon and change their bodies at the level of primary biochemical, cellular, molecular processes like ribosomic protein synthesis. Nikolas Rose (2007) has argued that this leads to entirely new forms of somatic (bodily) existence and genetic risk in which people come to define themselves by their genetic markers. People seek to not only cure illness or forestall congenital dispositions to disease but to optimize their existence through genetic engineering, designer pharmaceuticals, and epigenetic therapies.
Making Connections: Big Picture
The Biopolitics of Infectious Disease
Michel Foucault describes the history of Western society’s response to infectious disease in terms of three different biopolitical models of control: the exclusion of the sick, the discipline and rehabilitation of the sick, and the management of risks posed by the sick (Sarasin, 2020). Historically, these three models emerged in response to three different types of infectious disease: leprosy, plague, and smallpox. Biopolitical implications for the organization of modern societies, however, extend far beyond the response to illness.
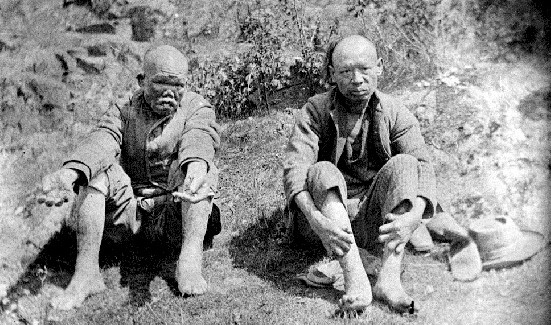
Leprosy (from the Greek for “scaly man”) is caused by the transmission of a bacteria that causes damage to the nerves, respiratory tract, skin, and eyes. In medieval Europe, people with leprosy, then referred to as “lepers”, were thought to be unclean and morally corrupt. They were segregated from society in infirmaries or leprosaria, or expelled beyond city limits and abandoned. Leper colonies, like D’Arcy Island near Victoria, BC, were maintained even into the 20th century. Foucault’s History of Madness (2006) describes how the model of excluding and confining people with leprosy began at the end of the middle ages to be more broadly applied, as a way to control the poor, vagabonds, the sick, and the mentally ill. These groups were interned together indiscriminately, without concern for dealing with or recognizing their distinct issues and needs. The leprosaria became the first houses for the poor, while also functioning as mental asylums. The term “mental asylum” refers to an inpatient psychiatric hospital for people living with mental illness, and may be offensive today. The exclusionary response to leprosy characterizes a model of power that separates deviants from “normals,” or the sick from the healthy, and abandons them outside society’s care.
In early modernity, the response to the bubonic plague provided a new model of control, which Foucault (1979) refers to as disciplinary power (see Chapter 8. Deviance, Crime and Social Control). Plague victims were no longer simply excluded and abandoned, but quarantined. To control the spread of plague, cities and towns were locked down, and citizens were subjected to a system of continuous surveillance and inspection, strict control of movement, and confinement to their homes. The plague model included uninterrupted surveillance of the population, normalization to distinguish the sick from the healthy and restore them to health, and examination to make certain families were abiding by quarantine measures and not hiding sick family members. This became the model for modern disciplinary institutions, including the prison system, the school, the workplace, the hospital, and the military. Rather than simply exclude and abandon individuals, disciplinary power seeks to discipline, transform, or rehabilitate them through close observation, the development of specialized knowledges (like medicine, psychology, and sociology), and continuous correction of behaviour.
The third biopolitical model developed as a risk management approach to smallpox epidemics. Beginning in the 18th century, Europeans responded to smallpox by tabulating statistics on the occurrence of illness in the population and attempting to protect the population through inoculation. By the 19th century, this became the basis for public health measures (such as sanitation, medical campaigns, and public cleanliness) and vaccination programs. This differed from the lock-down approach of disciplinary power, because it sought to manage the risk of the disease in the entire population, leaving ordinary daily life intact as far as possible, and relied largely on the voluntary compliance of the public with inoculation measures.
As Foucault (2007) put it,
The fundamental problem [is not] the imposition of discipline, although discipline may be called on to help, so much as the problem of knowing how many people are infected with smallpox, at what age, with what effects, with what mortality rate, lesions or after-effects, the risks of inoculation, the probability of an individual dying or being infected by smallpox despite inoculation, and the statistical effects on the population in general. In short, it [is not] the problem of exclusion, as with leprosy, or of quarantine, as with the plague, but of epidemics and the medical campaigns that try to halt epidemic or endemic phenomena.
In other words, the risk management model of social control, developed in the case of smallpox, attempts to manage the risk of a disease in the general population, while not undermining people’s freedom, which social systems rely on to operate effectively. Only in the most severe outbreaks did it resort to local disciplinary measures and quarantine.
Sarasin (2020) notes that Foucault’s three models of biopower can be used to study the implications of the responses to the COVID-19 pandemic:
- There are transitions and overlaps between the different forms of power. The complete lockdown of Wuhan rigorously followed the plague model, and every curfew ultimately does so, too. Only when systematic tests supply massive amounts of data about infected and non-infected people, as occurred in South Korea or Singapore, was it possible for governments to transition to the risk management model. Then they could restrict themselves to isolating the infected and recommend caution for the rest of the population, without however having to impose a lockdown.
- The plague model remains a danger to societies based on constitutional freedoms. Emergency measures that suspend ordinary laws and rights were used in many jurisdictions, including Canada, and once used the danger is that these could be extended or used more easily and frequently in the future. Moreover, the storage and evaluation of movement data of everyone carrying a mobile phone in some areas during the crisis expands the capacity of surveillance technology, which could be put to disciplinary purposes at a future date.
- The smallpox or risk management model of power was the dominant form of control used in North America and Europe, despite the differences between types of government. The strategy to “flatten the curve,” for example, is a risk management strategy that does not seek to eradicate the virus, but extends its distribution over time so that the health system can handle it. The strategies of wearing masks, prohibiting gatherings of several people, and the call to observe rules of “social distancing” were not disciplinary measures to control individual behaviour in a detailed and continuous way. They were narrowly focused, temporary social guidelines designed to decrease the risk of contagion while relying on voluntary compliance. While a collective means to manage risks, they rely on individuals taking the initiative to care for and protect themselves, but also create forms of neighbourly or solidary organization themselves.
- The leprosy model lurks in the background. It emerges in the occasional idea that we should let old people die “to save the economy,” or it becomes factual reality when retirement and nursing homes are abandoned, and their inmates die locked up and alone — as was reportedly the case in some homes in Ontario and Quebec in the early days of the COVID-19 pandemic.
Medical Sociology and the Social Construction of Health
The sociology of health encompasses social epidemiology, disease, mental health, disability, and medicalization. The principal insight of sociology is that health and illness cannot be simply regarded as biological or medical phenomena. They are perceived, organized, and acted on in a political, economic, cultural, and institutional context. Moreover, the way people relate to them is in constant evolution. As medical science learns to control existing diseases, new diseases develop. Similarly, as societies become global, the ways in which disease spreads evolve with them.
According to the World Health Organization (WHO), health “is a state of complete physical, mental and social well-being, and not merely the absence of disease or infirmity” (WHO, 2014). What does “health” mean to people? How does the WHO definition relate to contemporary issues of health? Are there too many people taking medications in Canadian society? Is there reason to be skeptical about people claiming they are “addicted” to gambling or “addicted” to sex? Are there historical diseases or conditions now considered within a spectrum of normality? Or are there conditions that have recently become known as a disease, but were previously considered evidence of laziness, moral weakness, or other character flaws? How do people decide whether children should receive vaccinations? These are questions examined in the sociology of health.
If sociology is the systematic study of human behaviour in society, medical sociology is the systematic study of how humans manage issues of health and illness, disease and disorders, and health care for both the sick and the healthy. Medical sociologists study the physical, mental, and social components of health and illness. Major topics for medical sociologists include the doctor-patient relationship, the structure and socioeconomics of health care, and how culture impacts attitudes toward disease and wellness.
The social construction of health is a major research topic within medical sociology. At first glance, the concept of a social construction of health may not make sense. After all, if disease is a measurable, physiological problem, then there can be no question of socially constructing disease, right? In fact, it is not that simple. The idea of the social construction of health emphasizes the socio-cultural aspects of the discipline’s approach to physical, objectively definable phenomena. Sociologists Conrad and Barker (2010) offer a comprehensive framework for understanding the major findings of the last 50 years of development in this concept. Their summary categorizes the findings in the field under three subheadings: the cultural meaning of illness, the social construction of the illness experience, and the social construction of medical knowledge.
The Cultural Meaning of Illness
Many medical sociologists contend that illnesses have both a biological and experiential component, and that these components exist independently of each other. Culture, not biology, dictates which illnesses are stigmatized, which are considered disabilities, and which are deemed contestable (meaning some medical professionals may find the existence of this ailment questionable) as opposed to definitive (illnesses that are unquestionably recognized in the medical profession) (Conrad and Barker, 2010).
For instance, sociologist Erving Goffman (1963) described how social stigmas hinder individuals from fully integrating into society. A stigma in general is defined by a “mark” of difference (e.g., a physiological “deformity,” personality “defect,” or status category like race, nationality, or religion) that defines a socially undesirable characteristic. Goffman elaborates:
an individual who might have been received easily in ordinary social intercourse possesses a trait that can obtrude itself upon attention and turn those of us whom he meets away from him, breaking the claim that his other attributes have on us (Goffman, 1963).
In other words, stigma works to define a person by a single attribute that makes them seem less than fully human and therefore subject to discriminatory practices, often unthinkingly. In meeting a stigmatized person, people construct a stigma theory that explains their inferiority and provides an account of the difference, threat, or danger they represent.
The stigmatization of illness often has the greatest effect on the patient and the kind of care they receive. Many contend that contemporary society and even health care institutions discriminate against certain diseases — like mental disorders, AIDS, venereal diseases, and skin disorders (Sartorius, 2007). Facilities for these diseases may be sub-par; they may be segregated from other health care areas or relegated to a poorer environment. This is a product of the stigma associated with the condition rather than the biology of the condition itself. As a result, the stigma may keep people from seeking help for their illness, making it worse than it needs to be.
Contested illnesses are those that are questioned or found questionable by some medical professionals. Disorders like fibromyalgia or chronic fatigue syndrome may be either true illnesses or only in the patients’ heads, depending on the opinion of the medical professional. This dynamic can affect how a patient seeks treatment and what kind of treatment they receive.
The Social Construction of the Illness Experience
The idea of the social construction of the illness experience is based on the concept of reality as a social construction. In this perspective, there is no objective reality independent of people’s own perceptions of it. The social construction of the illness experience deals with such issues as the way some patients control the way they reveal their disease, and the lifestyle adaptations patients develop to cope with their illnesses.
In terms of constructing the illness experience, culture, and individual personality both play a significant role. For some people, a long-term illness can have the effect of making their world smaller, more defined by the illness than anything else. For others, illness can be a chance for discovery, for re-imaging a new self (Conrad and Barker, 2010). Culture plays a huge role in how an individual experiences illness. Widespread diseases like AIDS or breast cancer have specific cultural markers that have changed over the years and that govern how individuals — and society — view them.
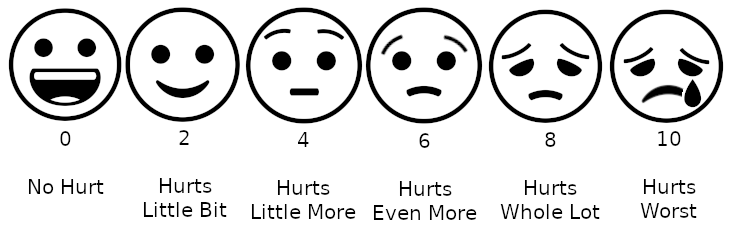
Today, many institutions of wellness acknowledge the degree to which individual perceptions shape the nature of health and illness. Regarding physical activity, for instance, the Public Health Agency of Canada recommends that individuals use a standard level of exertion to assess their physical activity. This rating of perceived exertion (RPE) gives a more complete view of an individual’s actual exertion level, since heart rate or pulse measurements may be affected by medication or other issues (CSEP, N.d.). Similarly, many medical professionals use a comparable scale for perceived pain to help determine pain management strategies.
The Social Construction of Medical Knowledge
Conrad and Barker (2010) show how medical knowledge is socially constructed; that is, it can both reflect and reproduce inequalities in gender, class, race, and ethnicity. They use the example of the social construction of women’s health and how medical knowledge has changed significantly in the course of a few generations. For instance, in the early 20th century, pregnant women were discouraged from driving or dancing for fear of harming the unborn child, much as they are discouraged from smoking or drinking alcohol today. Medical knowledge is used to reinforce ideas “about women’s ‘proper’ (i.e., subordinate) place in society, as well as moral assumptions about women’s sexuality and femininity more generally” (Conrad and barker, 2010).
Medicalization (discussed below in more detail) is also an aspect of the social construction of medical knowledge. Medicalization “occurs when human problems or experiences become defined as medical problems, usually in terms of illnesses, diseases, or syndromes” (Conrad and Barker, 2010). Again, the medicalization of Pre-Menstrual Syndrome (PMS) or menopause in women is an example in which natural reproductive functions of women are treated as disorders or medical conditions in need of medication. On the other hand, the renaming of male “impotence” as “erectile dysfunction” was part of medicalized branding exercise that coincided with the introduction of Pfizer’s pharmaceutical product Viagra. Originally targeted to older men, Pfizer quickly began promoting Viagra to a much larger audience as a means of enhancing male’s (or male partner’s) sexual experience, effectively medicalizing sexuality itself.
A social constructionist approach to medical knowledge provides a critical basis to examine how certain problems come to be defined in medical terms and how this translates into public policy.
Image Descriptions
Figure 19.5 long description: The Wong-Baker pain rating scale goes from 0 to 10. 0 is no pain, 2 is mild, 4 is discomforting, 6 is distressing, 8 is horrible and 10 is excruciating or the worst pain imaginable. The scale also used cartoon faces to illustrate the different levels of pain. 0 is smiling, 2 is a small smile, 4 is a straight face, 6 is a slightly sad face, 8 is a big sad face, 10 is a bigger sad face that is crying. [Return to Figure 19.5]
Media Attributions
- Figure 19.2 Me..Cyborg, by Donald Jusa, via Flickr, is used under a CC BY 2.0 licence.
- Figure 19.3 Andry tree by Nicolas Andry, via Wikimedia Commons, is in the public domain. Original from Orthopedics or the art of preventing and correcting deformities of the body in children, 1741, engraver unknown.
- Figure 19.4 Item D-04783 – Chinese Lepers At D’Arcy Island, circa 1890s from the BC Archives (Archives code(s): HP067703; 193501-001), via Royal BC Museum, is in the public domain.
- Figure 19.5 Emoji representation of the Wong–Baker Faces Pain Rating Scale for assessment of pain in children by Lord Belbury, via Wikimedia Commons, is used under a CC BY-SA 4.0 licence.

