Chapter 4. Wound Care
4.6 Moist to Dry Dressing, and Wound Irrigation and Packing
Moist to Dry Dressing
A moist to dry dressing is a primary dressing that directly touches the wound bed, with a secondary dressing that covers the primary dressing. The type of wound dressing used depends not only on the characteristics of the wound but also on the goal of the wound treatment.
Important: Ensure pain is well managed prior to a dressing change to maximize patient comfort.
Checklist 37 outlines the steps for performing a moist to dry dressing change.
Disclaimer: Always review and follow your hospital policy regarding this specific skill. |
|||
Safety considerations:
|
|||
Steps |
Additional Information |
||
| 1. Check present dressing using non-sterile gloves. | This provides an opportunity to collect required supplies for the procedure. | ||
| 2. Perform hand hygiene. | Hand hygiene reduces the risk of infection.
 |
||
| 3. Gather necessary equipment and supplies. | Being organized will help with efficiency and expedite the procedure, minimizing the length of time the patient experiences discomfort. | ||
| 4. Prepare environment, position patient, adjust height of bed, turn on lights. | This helps prepare patient and bedside for procedure. | ||
| 5. Perform hand hygiene. | Hand hygiene reduces the risk of infection.
 |
||
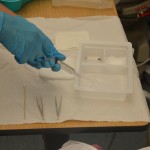
| 6. Prepare sterile field. |
 |
||
| 7. Add necessary sterile supplies. |
 |
||
| 8. Pour cleansing solution. |
 |
||
| 9. Expose dressed wound. | Inspect wound for the amount of drainage, odours, and type of drainage.
 |
||
| 10. Apply non-sterile gloves. | This reduces the risk of contaminating your hands with the patient’s blood and other body fluids.
It also reduces the risk of germ dissemination to the environment and of germ transmission from you to the patient and vice versa, as well as from one patient to another.  |
||
| 11. Remove outer dressing with non-sterile gloves. |
 |
||
| 12. Remove inner dressing with transfer forceps. |
 |
||
| 13. Discard transfer forceps and non-sterile gloves. |
 |
||
| 14. Drape patient with underpad (optional). |
 |
||
| 15. Apply non-sterile gloves (optional). | This reduces the risk of infection. | ||
| 16. Place sterile or non-woven gauze in container of prescribed solution, and wring out excess solution. | Use enough prescribed solution to saturate gauze. Excess solution has the potential to contaminate surrounding areas.
 |
||
| 17. Apply moist gauze as a single layer onto wound surface, pack gauze into wound if necessary, and ensure gauze does not touch skin around the wound. | Apply skin preparation as per agency protocol, if required.
 |
||
| 18. Cleanse around drain (if present). | Drain is cleansed using circular strokes starting near the drain and moving outward and away from the insertion site. | ||
| 19. Apply dry layer of sterile gauze over moist gauze using sterile technique. | This covers moist gauze and preserves moistness. | ||
| 20. Apply drain sponges/cut gauze to drain site if present. |
 |
||
| 21. Cover with ABD (abdominal) pad or gauze, and fasten with tape. | |||
| 22. Discard non-sterile gloves according to agency policy and perform hand hygiene. | Hand hygiene reduces the risk of infection.
 |
||
23. Next:
|
These steps ensure the patient’s continued safety. | ||
| 24. Document procedure and findings according to agency policy.
Report any unusual findings or concerns to the appropriate health care professional. |
Record dressing change: time, place of wound, wound characteristics, presence of staples or sutures, size, drainage type and amount, type of cleansing solution and dressing applied. | ||
| Data source: Perry et al., 2014; WHO, 2009 | |||
Wound Irrigation and Packing
Wound irrigation and packing refer to the application of fluid to a wound to remove exudate, slough, necrotic debris, bacterial contaminants, and dressing residue without adversely impacting cellular activity vital to the wound healing process (British Columbia Provincial Nursing Skin and Wound Committee, 2014).
Any wound that has a cavity, undermining, sinus, or a tract will require irrigation and packing. Open wounds require a specific environment for optimal healing from secondary intention. The purpose of irrigating and packing a wound is to remove debris and exudate from the wound and encourage the growth of granulation tissue to prevent premature closure and abscess formation (Saskatoon Health Region, 2013). Depending on the severity of the wound, it can take weeks to months or years to complete the healing process. Packing should only be done by a trained health care professional and according to agency guidelines.
Contraindications to packing a wound include a fistula tract, a wound with an unknown endpoint to tunnelling, a wound sinus tract or tunnel where irrigation solution cannot be retrieved, or a non-healing wound that requires a dry environment (Saskatoon Health Region, 2013).
The type of packing for the wound is based on a wound assessment, goal for the wound, and wound care management objectives. The packing material should fill the dead space and conform to the cavity to the base and sides. It is important to not over-pack or under-pack the wound. If the wound is over-packed, there may be excessive pressure placed on the tissue causing pain, impaired blood flow, and, potentially, tissue damage. If the wound is under-packed and the packing material is not touching the base and the sides of the cavity, undermining, sinus tract, or tunnel, there is a risk of the edges rolling and abscess formation (British Columbia Provincial Nursing Skin and Wound Committee, 2014).
The types of gauze used to pack a wound may be soaked with normal saline, ointment, or hydrogel, depending on the needs of the wound. Other types of packing material include impregnated gauze, ribbon dressing, hydro-fiber dressing, alginate antimicrobial dressing, and a negative pressure foam or gauze dressing. If using ribbon gauze from a multi-use container, ensure each patient has their own container to avoid cross-contamination (British Columbia Provincial Nursing Skin and Wound Committee, 2014). Additional guidelines to irrigating and packing a wound are listed in Table 4.6.
|
Guideline |
Additional Information |
||
| Aseptic technique | Sterile technique or no-touch technique may be used for irrigating and packing a wound. The use of a specific technique is based on agency policy, condition of the client, healability of the wound, invasiveness, and goal of the wound care. Sterile technique or no-touch technique must be used in all acute care settings. Clean technique may be used for chronic wounds in long-term-care settings. | ||
| Type of solution for irrigation | The most common solution used is normal saline at room temperature, unless otherwise ordered. Check physician orders. | ||
| Wound irrigation | The wound is irrigated each time the dressing is changed. | ||
| Irrigation pressure | The pressure of irrigating must be strong enough to remove debris but not damage the new tissue. Generally, a 35 ml syringe with a 19 gauge blunt tip is sufficient for irrigation. | ||
| Wound assessment | Wound assessment must be done with each dressing change to ensure the product is adequately meeting the needs of the wound. | ||
| Swabbing the wound | Swab for culture, if required. always swab a wound after irrigation. | ||
| Packing material | Packing material must be removed with each dressing change. Only one piece of gauze or dressing material should be used in wounds with sinus tracts or tunnelling to avoid the risk of retaining dressing/packing material. If there is a concern that packing is retained in the wound, contact the wound specialist or physician for follow-up.
Always leave a “tail” of the packing strip outside the wound. If more than one piece of packing is used, leave the tails outside the wound by securing the tails to the skin with a piece of Steri-Strip. |
||
| Documentation | Wound assessment and dressing change must be documented each time. Each wound requires a separate wound care sheet. Type and quantity of packing material (length or pieces), along with the number of inner and outer dressings should be recorded as per agency policy. For any cavity, undermining, sinus tract, or tunnel with a depth greater than 1cm (>1cm), count and document the number of packing pieces removed from the wound, and the number of packing pieces inserted into the wound. | ||
| Communication | A copy of the most recent wound care assessment and dressing change should be sent with patient upon transfer to another health care facility. | ||
| Use of sterile gloves for packing | Sterile gloves may be used if packing a large or complex wound. | ||
| Data source: British Columbia Provincial Nursing Skin and Wound Committee, 2014; Saskatoon Health Region, 2013 | |||
The health care professional chooses the method of cleansing (a squeezable sterile normal saline container or a 30 to 35 cc syringe with a wound irrigation tip catheter) and the type of wound cleansing solution to be used based on the presence of undermining, sinus tracts or tunnels, necrotic slough, and local wound infection.
Agency policy will determine the wound cleansing solution, but sterile normal saline and sterile water are the solutions of choice for cleansing wounds and should be warmed to support wound healing.
Undermining, sinuses, and tunnels can only be irrigated when there is a known endpoint. Do not irrigate undermining, sinuses, or tunnels that extend beyond 15 cm unless directed by a physician or nurse practitioner (NP). If fluid is instilled into a sinus, tunnel, or undermined area and cannot be removed from the area, stop irrigating and refer to a wound specialist or physician or NP.
Checklist 38 outlines the steps for irrigating and packing a wound.
Disclaimer: Always review and follow your hospital policy regarding this specific skill. |
|||
Safety considerations:
|
|||
Steps |
Additional Information |
||
| 1. Review order for wound irrigation and packing. | Confirm that physician’s orders are appropriate to wound assessment. | ||
| 2. Perform hand hygiene. | Hand hygiene reduces the risk of infection.
 |
||
3. Gather necessary equipment and supplies:
Some agencies provide a prepackaged sterile irrigation tray. |
Being organized will help with efficiency and expedite the procedure, minimizing the length of time the patient experiences discomfort.
 |
||
| 4. Position patient to allow solution to flow off patient.
Position patient so wound is vertical to the collection basin. |
 |
||
| 5. Place waterproof pad under patient.
Apply clean gloves. Set up sterile field and supplies. |
Protect patient’s clothing and bedding from irrigation fluid. | ||
6. Remove outer dressing.
|
 Removing packing that adheres to the wound bed without soaking can cause trauma to the wound bed tissue. If packing material cannot be removed, contact the physician / NP or wound clinician. If packing adheres to the wound, reassess the amount of wound exudate and consider a different packing material.  All packing must be removed with each dressing change. |
||
7. Assess the wound.
|
 Wound assessment helps identify if the wound care is effective. Always compare the current wound assessment with the previous assessment to determine if the wound is healing, delayed, worsening, or showing signs of infection. |
||
| 8. Apply non-sterile gloves, gown, and goggles or face shield according to agency policy. | The use of personal protective equipment (PPE) reduces the risk of contamination.
 |
||
| 9. Fill 35 to 60 ml syringe with sterile water/irrigating solution and attach a needleless cannula to end of syringe. |
 |
||
| 10. Hold syringe about 1 inch above wound and flush wound using gently continuous pressure until returns run clear into the basin.
If irrigating a deep wound with a very small opening, attach a small needleless catheter to prefilled irrigation syringe and insert about 1/2 inch. Use slow continuous pressure to flush wound. Repeat flushing procedure until returns run clear into the basin. |
 Irrigation should be drained into basin. Retained irrigation fluid is a medium for bacterial growth and subsequent infection. Irrigation should not increase patient discomfort. The irrigation tip controls the pressure of the fluid, not the force of the plunger. |
||
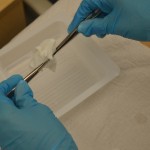
| 11. Dry wound edges with sterile gauze using sterile forceps. |
 This step prevents maceration of surrounding tissue from excess moisture. |
||
| 12. Remove goggles or face shield. | PPE is no longer required after irrigating a wound. | ||
| 13. Perform hand hygiene and apply sterile gloves (if not using sterile forceps) or non-sterile gloves. | Hand hygiene reduces the risk of infection.
 |
||
| 14. Apply a skin barrier / protectant on the peri-wound skin as needed. | Saturated packing materials and/or wound exudate may macerate or irritate unprotected peri-wound skin. | ||
15. For normal saline gauze packing:
|
The wound must be moist, not wet, for optimal healing. Gauze packing that is too wet can cause tissue maceration and reduces the absorbency of the gauze.
 Normal saline gauze packing needs to be changed at least once daily. If it is necessary to use more than one ribbon packing piece, the pieces must be tied together using sterile gloves; ensure the knot(s) is secure. Ensure the wound is not over-packed or under-packed as this may diminish the healing process.  This prepares the wound bed for optimal healing with a moist to dry dressing. |
||
| 16. Open gauze and gently pack it into wound using either forceps or the tip of a cotton swab stick. | Continue until all wound surfaces are in contact with gauze.
 Do not pack too tightly. Do not overlap wound edges with wet packing. |
||
| 17. Always leave a “tail” of packing materials either clearly visible in the wound cavity or on the peri-wound skin.
Use a Steri-Strip to secure the packing tail to the peri-wound skin. If two or more packing pieces have been knotted together, ensure that the knots are placed in the wound cavity, not in the undermining, sinus tract, or tunnel. |
 If the knot is visible in the wound, it is less likely that a packing piece will be lost if the knot comes undone. A knot exerting pressure on the wound surface may impair blood flow and potentially cause necrosis in the wound. |
||
| 18. Apply an appropriate outer dry dressing, depending on the frequency of the dressing changes and the amount of exudate from the wound. | The dressing on the wound must remain dry on the outside until the next dressing change to avoid cross-contamination of the wound.
 |
||
| 19. Discard supplies and perform hand hygiene. | This prevents the transfer of microorganisms.
 |
||
| 20. Help patient back into a comfortable position, and lower the bed. | This step optimizes patient safety. | ||
| 21. Document wound assessment, irrigation solution, and patient response to the irrigation and dressing change.
Documentation should include date and time of procedure. Report any unusual findings or concerns to the appropriate health care professional. |
This allows for effective communication between health care providers.
Notify required health care providers if wound appears infected or is not healing as expected. |
||
| Data source: BCIT, 2010b; Perry et al., 2014 | |||
Video 4.5
The following links provide additional information about wound packing and wound measuring.
Critical Thinking Exercises
- What information is documented when a wet to dry dressing change is performed?
- What temperature should the wound cleansing solution be?

