Chapter 4. Wound Care
4.2 Wound Healing and Assessment
Wound healing is a dynamic process of restoring the anatomic function of living tissue. Since damage to the body’s tissue is common, the body is well adapted to utilizing mechanisms of repair and defence to elicit the healing process. Normal wound healing is profoundly influenced by the type of injury and by factors about the wound (intrinsic) and within the patient (extrinsic) (Perry, Potter, & Ostendorf, 2014).
Phases of Wound Healing
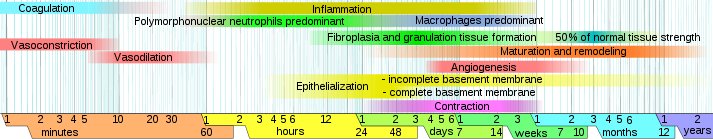
There are four distinct phases of wound healing. These four phases must occur in correct sequence and in a correct time frame to allow the layers of the skin to heal (see Figure 4.1). Table 4.1 describes how a wound heals.
|
Phase |
Additional Information |
||
| Hemostasis phase | Blood vessels constrict and clotting factors are activated. Clot formation blocks the bleeding and acts as a barrier to prevent bacterial contamination. Platelets release growth factors, which alert various cells to start the repair process at the wound location. | ||
| Inflammatory phase | Vasodilation occurs, allowing plasma and leukocytes (white blood cells) into the wound to start cleaning the wound bed. This process is seen as edema, erythema, and exudate. Macrophages (another type of white blood cell) work to regulate the cleanup. | ||
| Proliferative phase | Four important processes occur in this phase:
|
||
| Maturation (remodelling) phase | Collagen continues to strengthen the wound, and the wound becomes a scar. | ||
| Data source: British Columbia Provincial Nursing Skin and Wound Committee, 2011; Perry et al., 2014 | |||
Types of Wounds
To determine how to treat a wound, consider the etiology, amount of exudate, and available products to plan appropriate treatment. Wounds are classified as acute (healing occurs in a short time frame without complications) or chronic (healing occurs over weeks to years, and treatment is usually complex). Examples of acute wounds include a surgical incision or a traumatic wound (e.g., a gunshot wound). Examples of chronic wounds include venous and arterial ulcers, diabetic ulcers, and pressure ulcers. Table 4.2 lists the six main types of wounds.
|
Type |
Additional Information |
||
| Surgical | Healing occurs by primary, secondary, or tertiary intention.
Primary intention is where the edges are sutured or stapled closed, and the wound heals quickly with minimal tissue loss. The healing time for a surgical wound is usually short, depending on the surgery. A surgical wound left open to heal by scar formation is a wound healed by secondary intention. In this type of wound, there is a loss of skin, and granulation tissue fills the area left open. Healing is slow, which places the patient at risk for infection. Examples of wounds healing by secondary intention include severe lacerations or massive surgical interventions. Healing by tertiary intention is the intentional delay in closing a wound. On occasion, wounds are left open (covered by a sterile dressing) to allow an infection or inflammation to subside. Once the wound is closed with staples or sutures, the scarring in minimal. |
||
| Traumatic | Examples are gunshot wounds, stab wounds, or abrasions. These wounds may be acute or chronic. | ||
| Diabetic/neuropathic ulcer | This is a nerve disorder that results in the loss or impaired function of the tissues affecting nerve fibres. These wounds generally occur as a result of damage to the autonomic, sensory, or motor nerves and have an arterial perfusion deficit. They are usually located in the lower extremity on the foot. Diabetic/neuropathic ulcers are often small with a calloused edge. Pain may be absent or severe depending on the neuropathy. | ||
| Arterial ulcer | Arterial ulcers occur when tissue ischemia occurs due to arterial insufficiency from the narrowing of an artery by an obstruction (atherosclerosis). They are located on the distal aspects of the arterial circulation, and can be anywhere on the legs, including feet or toes. Wound margins are well defined with a pale wound bed with little or no granulation. Necrotic tissue is often present. There is minimal to no exudate present. Pedal pulses are usually absent or diminished. Pain occurs in limb at rest, at night, or when limb is elevated.
Arterial ulcers account for 5% to 20% of all leg ulcers. Perfusion must be assessed prior to initiating treatment. |
||
| Venous ulcer | A venous ulcer is a lower extremity wound. Tissue ischemia occurs due to the failure of the venous valve function to return blood from the lower extremities to the heart. It is usually located in the ankle to mid-calf region, usually medial or lateral, and can be circumferential. Drainage can be moderate to heavy. A venous ulcer can be irregularly shaped, large, and shallow with generalized edema to lower limbs. Pulse may be difficult to palpate.
Venous ulcers account for 70% to 90% of all leg ulcers. Perfusion must be assessed prior to initiating treatment. |
||
| Pressure ulcer | Also known as a pressure sore or decubiti wound, the pressure ulcer is a localized area of tissue damage that results from compression of soft tissue between a hard surface and a bony prominence (coccyx, ankle, shoulder blade, or hip). As blood supply decreases to the area of compression, tissue anoxia occurs, which can lead to eventual tissue death. Wounds are usually circular and may have viable or necrotic tissue, and exudate can vary from none to heavy. Pressure ulcers are classified depending on the level of tissue damage (stages 1 to 4). Treatment is based on stage, exudate, type of available dressing, and frequency of dressing changes. | ||
| Data source: British Columbia Provincial Nursing Skin and Wound Committee, 2011, 2014; Perry et al., 2014 | |||
Wound Healing
Wounds require different treatment throughout the phases of healing. There are multiple factors that affect how a wound heals as it moves through the phases of healing. It is important to look at the “whole patient” rather than the “hole in the patient” to identify the correct treatment and work efficiently and effectively from the beginning of the healing process.
Table 4.3 lists a number of factors that inhibit the ability of tissues and cells to regenerate, which can delay healing and contribute to wound infections.
|
Influencing Factors |
Additional Information |
||
| Patient’s age | Vascular changes occur with increasing age, skin is less pliable, and scar tissue is tighter.
For example, an older adult’s skin tears more easily from mechanical trauma such as tape removal. |
||
| Patient’s nutritional status | Tissue repair and infection resistance are directly related to adequate nutrition.
Patients who are malnourished are at increased risk for wound infections and wound infection-related sepsis. |
||
| Patient’s size | Inadequate vascularization due to obesity will decrease the delivery of nutrients and cellular elements required for healing.
An obese person is at greater risk for wound infection and dehiscence or evisceration. |
||
| Oxygenation | Factors such as decreased hemoglobin level, smoking, and underlying cardiopulmonary conditions will decrease oxygenation.
Adequate oxygenation at the tissue level is essential for adequate tissue repair. Hemoglobin level and oxygen release to tissues is reduced in smokers. |
||
| Patient’s medications | Steroids reduce the inflammatory response and slow collagen synthesis.
Cortisone depresses fibroblast activity and capillary growth. Chemotherapy depresses bone marrow production of white blood cells and impairs immune function. |
||
| Chronic diseases or trauma | Chronic diseases and traumas such as diabetes mellitus or radiation decrease tissue perfusion and oxygen release to tissues. | ||
| Data source: Gallagher-Camden, 2012; Perry et al., 2014; Stotts, 2012 | |||
Wound Assessment
Frequent wound assessment based on the type, cause, and characteristics of the wound is necessary to help determine the type of treatment required to manage the wound effectively and to promote maximal healing. The health care professional should always compare the wound to the previous assessment to determine progress toward healing. If there has been no improvement in the healing of the wound, alternative options or consulting a wound care specialist should be considered.
Checklist 32 outlines the steps to take when assessing a wound.
Disclaimer: Always review and follow your hospital policy regarding this specific skill. |
|||
Steps |
Additional Information |
||
| 1. Location | Note the anatomic position of the wound on the body. | ||
| 2. Type of wound | Note the etiology (cause) of the wound (i.e., surgical, pressure, trauma).
Common types are pressure, venous, arterial, or neuropathic/diabetic foot ulcers, or surgical or trauma wounds. |
||
| 3. Extent of tissue involvement | A full-thickness wound involves both the dermis and epidermis.
A partial-thickness wound involves only the epidermal layer. If the wound is a pressure ulcer, use the Braden Scale Interventions Algorithm. |
||
| 4. Type and percentage of tissue in wound base | Describe the type of tissue (i.e., granulation, slough, eschar) and the approximate amount. | ||
| 5. Wound size | Follow agency policy to measure wound dimensions, including width, depth, and length.
Assess for a sinus tract, tunnelling, or induration. |
||
| 6. Wound exudate | Describe the amount, colour, and consistency:
|
||
| 7. Presence of odour | Note the presence or absence of odour. The presence of odour may indicate infection. | ||
| 8. Peri-wound area | Assess the temperature, colour, and integrity of the skin surrounding the wound. | ||
| 9. Pain | Assess pain using LOTTAARP. | ||
| Data source: British Columbia Provincial Nursing Skin and Wound Committee, 2014; Perry et al., 2014 | |||
Critical Thinking Exercises
- Your patient is 75 years old, smokes cigarettes, has renal disease, and is overweight. What additional factors should you consider prior to assessing the patient’s wound?
- What phase of wound healing is indicated by the presence of epithelialization and wound contraction?
Attribution
Figure 4.1
Phases of wound healing by Mikael Häggström is in the public domain.