Chapter 9. Blood Glucose Monitoring
9.2 Glucometer Use
People with diabetes require regular monitoring of their blood glucose to help them achieve as close to normal blood glucose levels as possible for as much of the time as possible. The benefits of maintaining a blood glucose level that is consistently within the range of 4-7 mmol/L will reduce the short-term, potentially life-threatening complications of hypoglycemia as well as the occurrence rate and severity of the long-term complications of hyperglycemia.
Patients in the hospital setting are likely to have inconsistent blood glucose levels as they are affected by changes in diet and lifestyle, surgical procedures, and the stress of being in a hospital. The physician will prescribe how regularly the blood glucose should be monitored. In acute situations, a sliding-scale treatment for insulin will be individually prescribed per patient. The medication administration record (MAR) or sliding scale will provide directions for the amount of medication to be given based on the blood glucose reading.
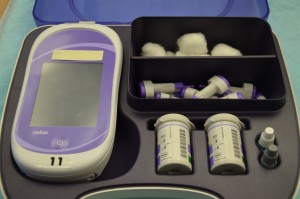
It is usually the responsibility of the nurse to perform blood glucose readings. As with any clinical procedure, ensure that you understand the patient’s condition, the reason for the test, and the possible outcomes of the procedure. Prior to performing a blood glucose test, ensure that you have read and understood the manufacturer’s instructions and your agency’s policy for the blood glucose monitoring machines (see Figure 9.1) used in your clinical setting, as these vary. It is also important that you determine the patient’s understanding of the procedure and the purpose for monitoring blood glucose level. Before you begin, you should also determine if there are any conditions present that could affect the reading. For example, is the patient fasting? Has the patient just had a meal? Is the patient on any medications that could affect the reading (e.g., anticoagulants)? In these situations, draw on your knowledge and understanding of diabetes, the medication you are administering, the uniqueness of your patient, and the clinical context. Use your knowledge and critical thinking to make a clinical judgment.
Inspect the area of skin that will be used as the puncture site and ask the patient if they are in agreement with the site you have identified to use for the skin puncture. Your patient may have a preference for the puncture site. For example, some patients prefer not to use a specific finger for the skin puncture. Or a particular site may be contraindicated. For example, you shouldn’t use the hand on the same side as a mastectomy.
Patients who do their own blood glucose testing at home may prefer to handle the skin-puncturing device themselves and continue self-testing while they are in the hospital.
Checklist 77 outlines the steps for taking a skin-puncture blood sample and using a blood glucose monitor (glucometer) to measure a patient’s blood glucose level.
Converting to Canadian (SI) measurements
Many nursing resources are from the United States, where glucose values are reported as mg/dl. Canadian laboratories use the international system of units (SI), which are mmol/L. Therefore, it is important to convert your patient’s laboratory values to SI units. For glucose, divide the mg/dl by 18 to find the comparable SI unit (e.g., 65 mg/dl = 3.61 mmol/L). This conversion chart shows specific conversions.
Blood Glucose Readings that Require Follow-up
The concerns listed in Table 9.1 must be attended to and reported immediately to the relevant health care provider. Please consult hospital/unit-specific recommendations for exact values. The concerns and actions in Table 9.1 are guidelines only.
| Concern | Action |
| Blood sugar outside “acceptable range” (<2.2 mmol/L or >20 mmol/L) | Repeat capillary test to confirm, and report if reading remains out of range. |
| Blood sugar <2.2 mmol/L or >20 mmol/L | Order a stat blood glucose (venous sample) by laboratory staff and initiate hypoglycemia or hyperglycemia protocol according to agency policy. |
| Blood sugar <4 mmol/L | Initiate hypoglycemia protocol according to agency policy. |
| Preoperative blood sugar <4 mmol/L or >20 mmol/L | Call physician. |
| Post-operative blood sugar >13.5 mmol/L (acceptable post-operative range = 8-13 mmol/L) | Test urine for ketones. If positive, monitor urine ketones every 4 hours. |
| Data source: BCIT, 2015 | |
Critical Thinking Exercises
- Describe two methods for increasing blood flow to a patient’s finger prior to lancing the finger.
- What is one thing that you must wait for before administering rapid-acting insulin to a patient on your ward?















